-

Intellectual Disability – An Impairment for Life Satisfaction
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
1-1
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.11
Downloads:
Views:
Abstract: Quality of life and life satisfaction for people with intellectual disabilities have only been addressed in a systematic way since the late 1980’s. Historically these areas have been neglected in research as intellectual disability was dominantly viewed within a medical model. Hence, intellectual disability was addressed predominantly in relation to quality of medical treatment and quality of institutional care. With the concept of normalization emerging the early 1960’s a social model social of intellectual disability experienced a steady expansion in our societies, thus focusing more and more on the individual person. The social model of intellectual disability asked for changes in the lives of people with intellectual disability in areas like early childhood, education, job opportunities up to accommodation, leisure time activities and old age. Along with these new person centered conceptions models of quality of life and life satisfaction were coined and methodologies on how to assess these areas were developed. The presentation will depict milestones of these new approaches and the way in which social and environmental changes contributed to the increase of life satisfaction in people with intellectual disabilities and the way these factors interact with a good quality of life and a good mental health, with challenges still awaiting to be tackled in our European regions.
Abstract: Quality of life and life satisfaction for people with intellectual disabilities have only been addressed in a systematic way since the late 1980’s. Historically these areas have been neglected in research as intellectual disability was dominantly viewed within a medical model. Hence, intellectual disability was addressed predominantly in relation t...
Show More
-

Forensic Preventive Community Treatment
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
2-2
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.12
Downloads:
Views:
Abstract: Background: Four five ago, the project Preventive Community Treatment started at the Forensic Clinic of Ansbach District Hospital. The aim of the project is to provide professional forensic psychiatric treatment to those patients who have not yet committed a crime linked to a mental illness but show a high-risk profile to commit a severe crime in future (i.e. violence, sexual offences). In this connection, the project focuses on patients suffering from schizophrenia and/or severe personality disorder and has been, for the start, designed for four years. The team is multi-professional and consists of psychiatrists, psychologists, social workers, and nurses who are all trained forensically. This team provides risk assessments to patients who are referred by general practitioners, psychiatrists, or their families. Patients who are regarded being at high risk are treated and monitored voluntarily by offering continuous appointments and doing home visits. The aim of the project is to reduce possible future crime committed by high-risk psychiatric patients. The project was evaluated by a long-term examination of a control group from Erlangen District hospital regarding aggression, severity of illness, outcome etc. The results will show the effectiveness of preventive treatment for psychiatric ill patients with a high risk for violence. Possibilities of a nationwide implementation of the project will be suggested.
Abstract: Background: Four five ago, the project Preventive Community Treatment started at the Forensic Clinic of Ansbach District Hospital. The aim of the project is to provide professional forensic psychiatric treatment to those patients who have not yet committed a crime linked to a mental illness but show a high-risk profile to commit a severe crime in f...
Show More
-

Confluence Elements in the Psychopathology and Neurobiology of Schizophrenia
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
3-3
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.13
Downloads:
Views:
Abstract: In the light of recent development of neurosciences, multiple studies aim to establish brain dysfunctions linked to psychiatric disorders. Schizophrenia is a severe long-term mental illness and recent research identified neurobiological changes with psychopathological effects.
The dopamine hypothesis has been one of the most enduring theories dominating the etiopathogenesis of schizophrenia. This theory is supported by the efficacy and potency of many antipsychotic drugs acting on dopamine and on another neurotransmitter with effects on dopamine, the serotonin. The dopamine theory postulates a mesolimbic dopaminergic hyperactivity linked to positive symptoms and a prefrontal cortex dopaminergic hypoactivity causing negative and cognitive symptoms in schizophrenia. Multiple theories implicating dysfunctions of glutamate and GABA prefrontal neurons integrate the above-mentioned dopamine abnormalities.
Schizophrenia is also conceptualized as a disconnection syndrome, therefore a lack of coordination between different cortical regions is argued, with emphasis on cortico-thalamic circuits. The thalamo-cortical dysconnectivity implies decreased connections between thalamus and dorsolateral prefrontal cortex.
In order to control perceptive and cognitive processes, the GABA prefrontal neurons are synchronized in the γ frequency band (30-80 Hz). In schizophrenia, there is a disturbed synchronicity in γ band and an increased activity in θ band, consistent with a hyper polarization with reduced control function of the prefrontal cortex. Also, chronic stress is associated with an inappropriate immune activation. Stress may increase pro-inflammatory cytokine. The activated immune system in turn activates the enzyme indoleamine 2,3-dioxygenase (IDO) of the tryptophan/kynurenine metabolism which influences the serotonergic and glutamatergic neurotransmission.
Epigenetic mechanisms may stem for the environmental contributions to schizophrenia, too. DNA methylation or histone acetylation could imply an active or inactive transcription in the case of some well-known enzymes intervening in the pathophysiology of schizophrenia like BDNF, COMT, GAD1 or RELN gene.
According to the “theory of self” in schizophrenia the structures implicated in “sense of self” elaboration are ventral medial, dorsal medial prefrontal cortex, anterior and posterior cingulate cortex, superior temporal sulcus, inferior parietal cortex.
Abstract: In the light of recent development of neurosciences, multiple studies aim to establish brain dysfunctions linked to psychiatric disorders. Schizophrenia is a severe long-term mental illness and recent research identified neurobiological changes with psychopathological effects.
The dopamine hypothesis has been one of the most enduring theories domina...
Show More
-

When Virtual Becomes Reality
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
4-4
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.14
Downloads:
Views:
Abstract: E-health includes medical help, education of the patient and of the specialist, and facilitates multidisciplinary approaches. A growing body of evidence illustrates that the developing of e-health, especially in the area of psychiatry represents a new horizon growing the access to care, the adherence to treatment, the efficiency of psycho-education, the quality of life, and also diminishes the stigmatization which is still associated with the use of mental health facilities. Unfortunately, the development of legislation regarding e-health remains behind the evolution of technology and this presentation will look into examples of standards and procedures and the need to implement these into practice.
Another field approached in this presentation and which is rapidly evolving is the one of Virtual Reality (VR) as a useful tool for assessment, diagnosis and treatment of psychiatric disorders. VR is used to treat patients with anxiety disorders, especially phobia, but its use is expanding quickly into other areas of psychiatric disorders.
Finally, the presentation discusses the impressive opportunities that artificial intelligence may bring into psychiatric evaluation and care. This approach may offer specialists more objective instruments when assessing the risk factors, the severity, and evolution of mental disorders.
Abstract: E-health includes medical help, education of the patient and of the specialist, and facilitates multidisciplinary approaches. A growing body of evidence illustrates that the developing of e-health, especially in the area of psychiatry represents a new horizon growing the access to care, the adherence to treatment, the efficiency of psycho-education...
Show More
-

Mental Health in Workplace - Mobbing, Burnout, Workaholism, Occupational Stress
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
5-5
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.15
Downloads:
Views:
Abstract: Human adaptation to the specific requirements and increasing complexity of work is often difficult. Serious psychological, medical, social and financial costs are involved, really affecting the functionality and the efficiency of the individuals, of the work group and sometimes even of the company.
Each work group has a specific work pathology, in which are intertwined the mobbing and occupational stress, the burnout and workaholism, organization’s structural and communicational failures, implicit values and organizational myths. The result is a complex pathology of work which is difficult to manage.
Abstract: Human adaptation to the specific requirements and increasing complexity of work is often difficult. Serious psychological, medical, social and financial costs are involved, really affecting the functionality and the efficiency of the individuals, of the work group and sometimes even of the company.
Each work group has a specific work pathology, in w...
Show More
-

Psychiatry in Crisis: Epistemological and Ontological Concerns
Drozdstoy S. Stoyanov,
Vincenzo Di Nicola
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
6-6
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.16
Downloads:
Views:
Abstract: It is not merely a health crisis of resource scarcity or distribution, competing claims and practice models, or level of development from one country to another, but a deeper, more fundamental crisis about the very definition and the theoretical basis of psychiatry.
The kinds of questions that represent this crisis include whether psychiatry is a social science (like psychology or anthropology), whether it is better understood as part of the humanities (like philosophy, history and literature), or if the future of psychiatry is best assured as a branch of medicine (privileging genetics and neuroscience)? In fact, the question often debated since the beginning of modern psychiatry concerns the biomedical model so that part of psychiatry’s perpetual self-questioning is to what extent it is or is not a branch of medicine.
From psychiatry in crisis as a medical discipline to critical psychiatry casting for a new model, what will be the result? Will it be the end of psychiatry or its renaissance as something new and different, either as a more comprehensive theory and practice of human being or as a new branch of medicine called the neuroscience?
Abstract: It is not merely a health crisis of resource scarcity or distribution, competing claims and practice models, or level of development from one country to another, but a deeper, more fundamental crisis about the very definition and the theoretical basis of psychiatry.
The kinds of questions that represent this crisis include whether psychiatry is a so...
Show More
-

Forensic Psychology: Suicide Risk in Penitentiary
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
7-7
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.17
Downloads:
Views:
Abstract: The penitentiary establishes a complex universe, sometimes unpredictable, having specific rules and procedures, but also a psychopathology significantly different from other environments. Hetero-aggressive and self-aggressive tendencies are much more frequent in incarcerate individuals, due to the rigidity of the environment and the tough conditions of life and survival, but also because of the personality disorders of the criminals or their difficulties to adapt to this oppressive environment.
The use of the aggressiveness as a strategy of survival is as often as self-harming and suicide tendencies. Suicide thinking, decision-making and the transition to act (parasuicide or effective suicide) have other patterns than among the normal population.
Abstract: The penitentiary establishes a complex universe, sometimes unpredictable, having specific rules and procedures, but also a psychopathology significantly different from other environments. Hetero-aggressive and self-aggressive tendencies are much more frequent in incarcerate individuals, due to the rigidity of the environment and the tough condition...
Show More
-

Clinical Trials: How, When, Why, What for
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
8-8
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.18
Downloads:
Views:
Abstract: Background: The concepts behind clinical trials are ancient. “The Book of Daniel” (100 BC) chapter 1, verses 12 through 15, for instance, describes a planned experiment with both baseline and follow-up observations of two groups who either partook of, or did not partake of "the King's meat" over a trial period of ten days. Persian physician Avicenna, in “The Canon of Medicine” (1025 AD), gave similar advice for determining the efficacy of medical drugs and substances. (Curtis L. Meinert; Susan Tonascia, 1986.Clinical trials: design, conduct, and analysis. Oxford University Press, USA. p. 3. ISBN 978-0-19-503568-1.)
Aims: Are clinical studies necessarry?
Clinical trials are experiments or observations done in clinical research. Such prospective biomedical or behavioral research studies on human participants are designed to answer specific questions about biomedical or behavioral interventions. Clinical trials generate data on safety and efficacy. ("Clinical Trials". Bill and Melinda Gates Foundation. Retrieved January 2014).
They are conducted only after they have received health authority/ethics committee approval in the country where approval of the therapy is sought. These authorities are responsible for vetting the risk/benefit ratio of the trial – their approval does not mean that the therapy is 'safe' or effective, only that the trial may be conducted.
Method: Explain the History of Clinical Trials, from the the ancient times to modern times, define and explain the process of Clinical Trials, the facts and reality of the process, the clinical phases, and most of all, the importance of those.
Results and Discussion: Fake press scandals in Romania, generalized from maybe only one case of tempering, greatly affecting the understanding of the importance of Clinical Trials in Romania (quote from media: “Guinea pigs, unapproved drugs used, astronomical sums for the corrupt doctors, etc.”). In fact, Romania is situated at the bottom of the list as for the number of clinical studies conducted here, but, instead, with very good statistical results.
Conclusion: Clinical trials are crucial, and still the perception of the Romanian population, supported by the media, and not contradicted by the authorities, are that those are only “Guinea pigs studies”. This perception should be changed, and the ones that can do that are the Medical Doctors- and this presentation is one of those steps.
Abstract: Background: The concepts behind clinical trials are ancient. “The Book of Daniel” (100 BC) chapter 1, verses 12 through 15, for instance, describes a planned experiment with both baseline and follow-up observations of two groups who either partook of, or did not partake of "the King's meat" over a trial period of ten days. Persian physician Avicenn...
Show More
-

Through Attitude, Towards Fulfilment
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
9-9
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.19
Downloads:
Views:
Abstract: In a very sharp way of seeing daily reality I have the tendency of putting it like this: “Today, psychiatry is misdirected. Depression is not the main problem and will not be the biggest burden in the immediate future. Depression is a symptom of a bigger social problem. Personality disorder (PD) is the main problem and a reason for depression. On the other hand, psychiatry is powerless in relation with PD. It even has a tendency to bury the problem under the cultural particularity of a nation or of a social group. It seems, the natural development of the human being is becoming a burden, because of the lack of resources that psychiatry (society) has, in dealing (handling) with PD.” In e very peaceful, warm way of seeing daily reality I have the ground of putting it like this: “We are different. Our mind has a large variety in perceiving, understanding and answering to the world around. Some of us tend to decide on a problem, a question that we encounter, in a very sharp, rigid, way. Some tend to oscillate a lot. Many of us use this, two variations, in alternation, based on situation ground: (very) rigid at work, (very) oscillating with close ones or the other way around, as an example. One seems to have trust, power, the other doubt, and weakness.” We can very easily see these two decisions making mechanisms to dominate the psychopathic structure or the neurotic structure. What is very hard to see is the value of them both, the error we make when we understand them, when we give them o social meaning and secondary a social roll, a value. It is not a bad, an illness to be psychopath or neurotic, it is bad, wrong or ill the way we behave with that because we neglect the value of emotions, the need for active dedication in order to develop emotional maturity, consolidated feelings (sentiments) of trust (vertrauen), love (liebe), loyalty (treue) and their successor and consolidator: fulfilment (erfülung).
Abstract: In a very sharp way of seeing daily reality I have the tendency of putting it like this: “Today, psychiatry is misdirected. Depression is not the main problem and will not be the biggest burden in the immediate future. Depression is a symptom of a bigger social problem. Personality disorder (PD) is the main problem and a reason for depression. On t...
Show More
-

Non-voluntary Hospitalization of Patients with Mental Disorders in “SOCOLA” Institute of Psychiatry – Iasi, Romania
Petronela Nechita,
Georgiana Crăciun,
Mihai Mutica,
Oana Hanut,
Alexandru Bogdan Ciubară,
Mihai Pirlog,
Anamaria Ciubară
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
10-10
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.20
Downloads:
Views:
Abstract: Research shows that mental health legislation is seen as an event that occurs every few decades and not as a process. Laws on voluntary or non-voluntary hospitalization of patient with mental disorders in many European countries were reformed. But legislation that refers to non-voluntary hospitalization of patients with mental disorders differ between Member States of the European Union. In Romania, Law 487/2002 is the mental health and protection of people with mental disorders law. Also, Law 129/2012 amending and supplementing Law 487/2002 surprise us with new legislative developments designed to align us with European standards. Implementing mental health law republished occurred in May 2016. The purpose of this study is to highlight the ethical and legal aspects, but also bio-psycho-social, of non-voluntary patients hospitalized in the Institute of Psychiatry "Socola", Iasi. Material and methods: The study is quantitative, retrospective, and the data were processed from observation sheets of 265 patients non-voluntary hospitalized in “Socola” Institute of Psychiatry, according to the law 487/2002, but and after republishing law in July 2012. Results show differences between non-voluntary admissions by law 487/2002 vs. republished health law in July 2012. The group may be mainly described in the majority male, from urban environment, aged below 40 years, with discharge diagnosis from Schizophrenia or other psychotic disorders category. Non-voluntary hospitalization criteria according article 45/54, paragraph a), b) have been met. The application for non-voluntary hospitalization of patients with mental disorders came mostly from family. In conclusion, this many changes on health legislation cause psychiatrists to document permanently from a legal standpoint to make correct decisions and act quickly. Advance directives implementation in the legal system of mental health as an opportunity through which the patient can express his future wishes for psychiatric care (including non-voluntary hospitalization).
Abstract: Research shows that mental health legislation is seen as an event that occurs every few decades and not as a process. Laws on voluntary or non-voluntary hospitalization of patient with mental disorders in many European countries were reformed. But legislation that refers to non-voluntary hospitalization of patients with mental disorders differ betw...
Show More
-

Psycho-Endocrine Markers of Relapse Prediction in Alcohol Addiction
Ion V. Cosicug,
Victor N. Lacusta,
Inga D. Deliv,
Irina I. Padure
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
11-11
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.21
Downloads:
Views:
Abstract: Background: There are multiple psychological and endocrine factors which may provoke early relapses in alcohol dependent patients, but it is not known in which measure they correlate with the risk of alcohol dependence relapse.
Aims: To study the possibility of prognostication of early relapses in alcohol dependence, taking into account the correlation of various psycho-endocrine factors with the disease relapse risk.
Method: The design of the study was based on prospective and retrospective clinical and psychological exploration (to quantify the intensity: craving [CR] anxiety [ANX] dysphoria [DISF] depression [DEPR]) and radio-immunological methods of evaluation of the plasmatic level of hormones (adrenocorticotropic hormone (ACTH), prolactin (PRL), cortisol (F)). The complex analysis of data obtained by statistical methods (cluster analysis).
Results and Discussion: To assess the likelihood of early relapse in alcohol addiction were investigated clinically and laboratory results of 158 patients, being in the initial period of installed remission of alcohol dependency (the first 6 months after the anti-alcoholic treatment). Using a mathematical statistic method (cluster analysis) was studied how different factors correlate (emotional, and endocrine) with alcohol dependency risk of relapse. The complex analysis of data obtained by statistical methods (cluster analysis), has shown that the prognosis of early alcohol relapses is more efficient when a set of different factors is analyzed.
Conclusion:An efficient prognosis (in 66.07% of cases) can be obtained by the application of the formula of the discriminant function f = 19.61456 x (CR) 0.000101 x (ANX x PRL) 0.301934 x (ANX x CR) + 1, 8236 x (DISF x CR) x 4.13376, developed in the present study. Thus, the psycho-endocrine parameters: the plasma level of prolactin, anxiety, craving, dysphoria can be considered markers in relapse prediction in alcohol dependence.
Abstract: Background: There are multiple psychological and endocrine factors which may provoke early relapses in alcohol dependent patients, but it is not known in which measure they correlate with the risk of alcohol dependence relapse.
Aims: To study the possibility of prognostication of early relapses in alcohol dependence, taking into account the correlat...
Show More
-

The Effect of Pulmonary Rehabilitation on Psychological Status and Quality of Life
Alina Croitoru,
Daniela Jipa,
Andreea Dumitrescu,
Mihai Mutica,
Miron Bogdan
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
12-12
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.22
Downloads:
Views:
Abstract: Introduction: Patients with chronic respiratory diseases are suffering from dyspnea and decreased daily activity, which affects quality of life and psychological status. One of the objectives of pulmonary rehabilitation programs is to improve their psychological status.
Aim: to evaluate the benefits of pulmonary rehabilitation (PR) on level of anxiety and depression among patients included in a pulmonary rehabilitation program.
Method: A prospective study on COPD (Chronic obstructive lung disease) patients participating in a 7 weeks outpatient rehabilitation program that includes: generally physical training, chest physiotherapy, psychological counselling (one session / week). The following parameters were evaluated before and after RR: dyspnea (BORG scale), quality of life (St. George's Respiratory Questionnaire: SGRQ), psychological status (Hospital Anxiety and Depression Scale).
Results: 47 COPD patients, mean age 61.83±12.3 years, 37 males. Before the rehabilitation, we found in 38/47 patients anxiety and depression (HADS score>8 points), of which 35 had moderate and severe scores. After the RR program: mean dyspnoea score decreased from 2.6 to 1.8 points (BORG scale, p = 0.000, test Wilcoxon), improved quality of life (SGRQ score decreased from 52.3 to 47.1 points, p = 0.000, t student). Mean HADS value significantly decreased from 14.4 to 12.3 points, p=0.000, t student). The benefits on psychological status were higher in the age group > 65 years, severe functional COPD stages, women.
Conclusions: Our pulmonary rehabilitation program had statistically significant positive effects on dyspnea, quality of life and anxiety and depression in COPD patients. Psychological counselling added to muscular training increase the success rate of rehabilitation and the adherence to the program.
Abstract: Introduction: Patients with chronic respiratory diseases are suffering from dyspnea and decreased daily activity, which affects quality of life and psychological status. One of the objectives of pulmonary rehabilitation programs is to improve their psychological status.
Aim: to evaluate the benefits of pulmonary rehabilitation (PR) on level of anxie...
Show More
-

Strategies to Prevent Delirium in ICU
Mary-Nicoleta Lupu,
Alexandru Bogdan Ciubară,
Mădălina-Nina Sandu
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
13-13
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.23
Downloads:
Views:
Abstract: Delirium confusion state is a serious problem common in ICU especially in elderly patients (> 65 years), which can cause cognitive dysfunction in the short term and long term, increase the number of days of hospitalization worsening evolution, increasing the number of complications, and the levels of morbidity and mortality. The most important risk factors which determine the delirium are considered: visual disturbances, severe illness (pneumonia, chronic lung disease, congestive heart failure, unbalanced diabetes, cerebrovascular disease, etc.), cognitive impairment or dementia, dehydration, lack of sleep, impaired hearing. Numerous studies have shown that delirium prevention is more effective than treating it, stressing the importance of recognizing delirium assessment and staff training for its diagnosis. The implementation of such measures in intensive care units may help improve patient outcomes, shorten the stay in intensive care after discharge, avoiding the occurrence of disability.
Abstract: Delirium confusion state is a serious problem common in ICU especially in elderly patients (> 65 years), which can cause cognitive dysfunction in the short term and long term, increase the number of days of hospitalization worsening evolution, increasing the number of complications, and the levels of morbidity and mortality. The most important risk...
Show More
-

Prescribing Anticholinergic Medication in Neurocognitive Disorders: Pharmacological Implications and Clinical Proofs
Bogdan Mircea Petrescu,
Alina Mitrache,
Daniel Vasile,
Octavian Vasiliu,
Andrei Gabriel Mangalagiu,
Cristian Alexandru Cândea
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
14-14
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.24
Downloads:
Views:
Abstract: The use of anticholinergic medicines is a widespread practice in older adults. Numerous studies have emphasized that the use of anticholinergics can be associated with a high risk of developing dementia. The aim of this analysis is to describe pharmacologically the interactions and effects of the use of anticholinergics in neurocognitive disorders and to offer practical advice for limiting or even avoiding altogether using this type of medicines when the risks are greater than the benefits.
In conclusion, there is evidence suggesting that the anticholinergic medicines can increase the risk of dementia. Considering this potential risk and the multitude of well-known adverse effects (constipation, diplopia, urinary retention and delirium) associated with the anticholinergic medicines, it is prudent to limit their use and consider possible alternatives.
Abstract: The use of anticholinergic medicines is a widespread practice in older adults. Numerous studies have emphasized that the use of anticholinergics can be associated with a high risk of developing dementia. The aim of this analysis is to describe pharmacologically the interactions and effects of the use of anticholinergics in neurocognitive disorders ...
Show More
-

The Psychophysiological Effects of the Chemical Terrorist Attacks – the Neurotoxic Agent: Sarin
Bogdan Mircea Petrescu,
Daniel Vasile,
Octavian Vasiliu,
Andrei Gabriel Mangalagiu,
Mihai Alin Bădic
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
15-15
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.25
Downloads:
Views:
Abstract: Sarin (GB, O-Isopropyl methylphosphonofluoridate) is an organophosphate neurotoxic agent that inhibits irreversibly acetylcholinesterase (AChE). Next, the accumulation of acetylcholine (ACh) in the central nervous system (CNS) causes convulsions and, in high dosage, centrally mediated respiratory failure. The ACh accumulation at peripheral vegetative synapses level leads to peripheral signs of intoxication and overstimulation of muscarinic and nicotinic receptors, which is described as “cholinergic crisis” (diarrhea, perspiration, salivation, miosis, bronchospasm). The exposure to high dosage of Sarin may lead to tremor, convulsions and hypothermia. More seriously, the accumulation of ACh at neuromuscular junctions’ level may also cause paralysis and peripherally mediated respiratory failure that can lead to death by breathing arrest.
In addition to the main action on the cholinergic system, Sarin has other secondary effects. These involve activating some neurotransmitters including the gamma-amino-butyric acid (GABA) and alteration of other cellular signaling systems, such as the ionic channels, cellular adhesion molecules and inflammation regulators. The Sarin exposure is associated with symptoms of late neurotoxicity induced by organophosphates and chronic neurotoxicity induced by organophosphates. Moreover, Sarin has been involved in the toxic and immunotoxic effects such as endocrine disorders induced by organophosphates.
The standard treatment for exposure to the Sarin neurotoxin is a post-exposure injection with atropine, an antagonist of muscarinic receptors, followed by oxime, an AChE reactivator, and diazepam.
Abstract: Sarin (GB, O-Isopropyl methylphosphonofluoridate) is an organophosphate neurotoxic agent that inhibits irreversibly acetylcholinesterase (AChE). Next, the accumulation of acetylcholine (ACh) in the central nervous system (CNS) causes convulsions and, in high dosage, centrally mediated respiratory failure. The ACh accumulation at peripheral vegetati...
Show More
-

Mental Health Economics: Real Cost of Care
Florin M. Buhociu,
Valentin M. Antohi
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
16-16
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.26
Downloads:
Views:
Abstract: Introduction: Mental health or psychological has always been a significant part of what we call generic "human health", as a constant and major concern not only for those in charge of organizing healthcare systems, be they public or private, but for all which, in one way or another deal with the management of human factor. Of course, ensuring a mental health corresponding for every individual, member of society in which he lives, has major costs, economic and social. Our paper has proposed that, starting from the evolution of the Romanian population over the last 50 years, taking into account the outstanding statistics on mental disorders in the EU and Romania, to highlight the costs and sources of funding of mental health services in our country They were studied numerous specialized works, some of which were published in ISI magazines and ISI Proceedings in Europe and the US. There have also been analyzed reports of specialized agencies, such as Health Care Cost Institute also from US so that by comparison, we can identify the specific dynamics and forms of funding mental illness in Romania.
Method: Starting from mental health concepts, the authors identified and analyzed the main programmatic documents and organizational framework for assessing the state of health in Romania. So, they have analyzed the National Health Programs and the Strategy for Mental Health in Romania, aiming at evolution of funds allocated in recent years to this very important area. The statistical analysis of the data specific to the area studied allowed us to study the dynamics of the allocation of public and private funds to this sector of mental health over the last years.
Results and Discussion: Financing mental health services in Romania is either with funds from the Ministry of Health or from the National House of Health. Once Romania joined the EU in 2007 it began to be concerns for funding health projects from European Funds also. The authors have identified and presented some European Funds and Operational Programs which allow funding of public mental health services, focusing on the need to increase the share of this type of financing within the total costs. It has also been studied the experience of these health services in European countries and in the United States of America. Thus, they were identified and analyzed public health system costs for job loss or depression, a disease widespread in major corporations in these states. Also they have been studied the social costs of excessive use of social networks such as Facebook and mental health at the work place. We appreciate that studying simultaneously both health costs and social ones on health mental constitute a solution for knowledge, quantification and treatment of such diseases that have a high prevalence, especially in contemporary society.
Abstract: Introduction: Mental health or psychological has always been a significant part of what we call generic "human health", as a constant and major concern not only for those in charge of organizing healthcare systems, be they public or private, but for all which, in one way or another deal with the management of human factor. Of course, ensuring a men...
Show More
-

The Role of Psychosocial Intervention on the Course of the Disease in Persons with Severe Mental Disorders
Ana Popova,
Victoria Dobreva
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
17-17
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.27
Downloads:
Views:
Abstract: Background:Data from literature emphasized the role of different interventions during the evolution of mental health disorders, out of which psychosocial approach had proved its efficacy and efficiency.
Aims: The current study is covering the cases of 220 people with severe mental disorders, classified by International Classification of Diseases with the following diagnoses: F06.2, F06.3, F10.51, F11.5, F20.0, F20.6, F22.0, F23.1, F25.2, F30.2, F31.6, F32.1, F33.2. The age of the patients in the study is between 18 and 71. Their family status and support are the main criteria. The patients were having their compulsory treatment in psychiatric facilities in Sofia city and Sofia region. Within the period from 2013 to 2015, their use of the service of psychosocial rehabilitation and compulsory treatment has been monitored.
Method: The analysis was based on data collected from the medical reports of patients. The SPSS software was used for statistical processing of the collected data. The following methods (assays) are used in this study: descriptive statistics, frequency analysis; analysis of variance;
correlation analysis;
Results and Discussion: There are psychosocial and demographic factors for patients with mental disorder, which will be observed below. Some of them may affect the treatment of the patients.
Conclusion:The results obtained using variance analysis support the hypothesis that there is a difference between the number of rehospitalizations and the number of conducted psychosocial rehabilitations. The assumption that there is a difference in the number of re-hospitalizations due to factors such as disability, age, diagnosis, education, family status, has not been confirmed in the present study, which can only emphasize the significance and importance of the psychosocial rehabilitation.
Abstract: Background:Data from literature emphasized the role of different interventions during the evolution of mental health disorders, out of which psychosocial approach had proved its efficacy and efficiency.
Aims: The current study is covering the cases of 220 people with severe mental disorders, classified by International Classification of Diseases wi...
Show More
-

Clinico-psychological and Psychopathological Aspects of Schizophrenia and Homicide
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
18-18
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.28
Downloads:
Views:
Abstract: Background: The problem of homicide in mental illness, and particularly in schizophrenia, is crucial for a broad spectrum of scientific disciplines.
Aims:To explore clinical and psychological and psychopathological characteristics of a group of schizophrenic patients, who committed homicide.
Method: Experimental group encompassed 47 patients with schizophrenia and homicide, first control group included 50 age and education matched controls with schizophrenia and a second control group without schizophrenia, but with homicide. All patients were assessed by PANSS, Rosenzweig frustration tolerance test, GAF and Buss-Durkee hostility questionnaire.
Results and Discussion: In general, patients with schizophrenia and homicide were more severely ill in comparison with the control group. The item “unusual thought content” correlated significantly with homicide in schizophrenia.
Conclusion: Most of the symptoms were more prominent in patients with schizophrenia and homicide. Some differences were found. Further studies are needed to explain pathophysiological and patho-plastic aspects.
Abstract: Background: The problem of homicide in mental illness, and particularly in schizophrenia, is crucial for a broad spectrum of scientific disciplines.
Aims:To explore clinical and psychological and psychopathological characteristics of a group of schizophrenic patients, who committed homicide.
Method: Experimental group encompassed 47 patients with sch...
Show More
-

The Conundrum of Prolonged Delirium Tremens
Ionuţ D. Rădulescu,
Elena Stoenescu,
Radu Andrei
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
19-19
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.29
Downloads:
Views:
Abstract: Introduction: Delirium tremens (DTs) is the most severe form of ethanol withdrawal manifested by altered mental status with disturbances of cognition, perception, sensorium and by sympathetic overdrive with autonomic hyperactivity, disturbances in alertness, sleep/wake cycles and psychomotor behavior, which can progress to cardiovascular collapse. DT’s is a medical emergency with a high mortality rate, making early recognition and treatment essential.
Material and methods: Case Report: A 60 year old male with past medical history of type 2 diabetes and alcohol dependence was admitted to the hospital with a confusional state, tremor of the extremities, faintness, dysthymia with emotional instability symptoms, linked to alcohol consumption. The patient status under specific treatment with: intravenous (IV) rehydration, vitamin supplements of thiamine, oral and IM Diazepam and oral Haloperidol showed only slight improvement in the first days before his confusional state got worse and starting having headaches. Due to this fact a CT scan was indicated. A contrast-enhanced cranial CT revealed a tumor situated in the left parietal-occipital lobes and in the corpus callosum bilateral. He was redirected to a Neurosurgery clinic for further investigation where a biopsy was taken diagnosing a stage 4 glioblastoma.
Results and discussion: Alcohol withdrawal delirium is usually short-lived and lasts for approximately 3 days in most cases. Rarely, it may persist for a longer period of time prompting a search for other contributing factors. In the case of our patient his cognitive impairment, confusion, memory and sleep problems, sluggishness, drowsiness, changes in emotional state where more general, nonspecific symptoms of a brain tumor. This coupled with his unreliable testimony about his drinking habits, absence of a head trauma or withdrawal seizures and the fact that our clinic had no CT equipment at that time, made the differentiating between the two diagnosis difficult in the beginning.
Disclosure: I declare that there are no conflicts of interest or support that may cause bias in my presentation.
Abstract: Introduction: Delirium tremens (DTs) is the most severe form of ethanol withdrawal manifested by altered mental status with disturbances of cognition, perception, sensorium and by sympathetic overdrive with autonomic hyperactivity, disturbances in alertness, sleep/wake cycles and psychomotor behavior, which can progress to cardiovascular collapse. ...
Show More
-

Psychotropic Drugs and the Risk of Fracture in Old Age
Viorel Oltenacu,
Paul Dan Sîrbu,
Razvan Tudor,
Alexandru Bogdan Ciubară,
Roxana-Cristina Damaschin,
Anamaria Ciubară
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
20-20
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.30
Downloads:
Views:
Abstract: Introduction Fractures in old age is a major health problem with considerable disability and mortality. Antipsychotic drugs (APs) have been associated with falls and fractures in elderly individuals.
Methods The study performed was a retrospective analysis with 97 participants. Subjects were everyone over the age of 65 with fractures radiologically confirmed, hospitalized in Department of Orthopaedics and Traumatology “Sf. Ap. Andrei” Galaţi, România, in May 2017. The objective was to evaluate the association between APs and the risk of fractures in elderly persons.
Results and discussion16 participants with confirmed fracture (16.50%) was associated with exposure to psychotropic medications. Those who took selective serotonin reuptake inhibitors (SSRIs), in particular, are linked to greater susceptibility to bone fractures: 10 out of 16 participants.
Conclusion The mechanism leading to this increased risk is unclear. Clinical studies examining causality or mechanisms of the observed association between antipsychotic drug use and excess risk of fractures are needed. Confounding by indication, other drugs used or comorbidity cannot be excluded, this association is relevant for clinical practice because fractures and antipsychotic drug use are prevalent in vulnerable older individuals.
Abstract: Introduction Fractures in old age is a major health problem with considerable disability and mortality. Antipsychotic drugs (APs) have been associated with falls and fractures in elderly individuals.
Methods The study performed was a retrospective analysis with 97 participants. Subjects were everyone over the age of 65 with fractures radiologically ...
Show More
-

Prevention of Depression and Anxiety in Primary Health Care
Rumiana Dinolova-Hodgadgikova,
Hristo Hinkov,
Zahari Zarkov,
Vaska Stancheva-Popkostadinova
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
21-21
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.31
Downloads:
Views:
Abstract: Depression and anxiety disorders are the most common mental disorders in our society. Some recent studies claim that 11.4 % of Bulgarians suffer from anxiety disorders, and 6.2%-from depressive disorders.
The objectives of the paper is to present the results of the awareness raising and training in mental health professionals for dealing with depression and anxiety in the frame of the project “Improved mental health services”, funded by EEA and Norway grants’ scheme.
The training consists of 2 parts. The first stage aims to increase knowledge of General practitioners, psychologists and social workers in early identification and interventions in anxiety disorders and depression in primary practice. The training was developed and implemented in 2 stages. The training through the first stage was conducted in a form of electronic course. In advance electronic portal was particularly developed for the purposes of the project. As for the second stage of the training, 3-day face-to-face workshops were organized. Furthermore, a Manual for helping professions for early identification of depression and anxiety in primary health care was written and distributed to the participants.
A total of 2500 general practitioners, psychologists and social workers from South-West, South Central and North central regions of Bulgaria registered in the electronic platform for the specialized training, however, 2300 completed the training (1300 completed only the online training, while 1000 completed both stages of the training).
The aim of the second part of the training was to prepare 53 experts within 28 Regional Health inspections from all over the country for implementation of programs for primary and secondary suicide prevention in schools. Interactive workshops with duration of 3 days were organized.
Educational materials with stress on anxiety, depression, aggression, self-harm behaviour, sexual health was developed for the population of students from 8th to 11th grades. Moreover, on the website of the project are available booklets on depression, anxiety, violence and suicide prevention, as well as guidelines for teachers on how to talk to their students on these topics.
The outcomes of the practitioners’ training from primary health care practice and Regional health inspections are discussed in the framework of existing and relevant legislation and professional standards and possibilities for future dissemination and sustainability.
Abstract: Depression and anxiety disorders are the most common mental disorders in our society. Some recent studies claim that 11.4 % of Bulgarians suffer from anxiety disorders, and 6.2%-from depressive disorders.
The objectives of the paper is to present the results of the awareness raising and training in mental health professionals for dealing with depres...
Show More
-

Psychological Morbidity Associated with Orthopedic Trauma
Razvan Tudo,
Viorel Oltenacu,
Paul Dan Sîrbu,
Anamaria Ciubară,
Roxana-Cristina Damaschin,
Alexandru Bogdan Ciubară
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
22-22
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.32
Downloads:
Views:
Abstract: Little is known about the clinical consequences of psychological morbidity associated with orthopedic trauma. Previous work has reported that mental illness is an independent predictor of poor outcome following orthopedic trauma, and future studies should explore whether management of psychological symptoms independently predicts recovery from orthopedic trauma. Anxiety disorders, depression, bipolar disorder, schizophrenia, and personality disorders may all flare up during the post-operative period, leading to psychiatric consultation. Other common general post-operative issues include complications related to alcohol abuse, dependence, and withdrawal; pain management in opioid-dependent patients; the presence of personality disorders and other causes of lack of cooperation; and post-operative delirium. Posttraumatic stress disorder (PTSD) is also common after surgery, particularly after traumatic injuries, but is underrecognized and undertreated. Previous research has evaluated these and other issues in surgical patients. Although psychiatric problems are seen less frequently than previously, the orthopaedic surgeon must remain aware of their possible effect. The prevalence of psychological illness following traumatic injuries varies according to the diagnostic criteria used in studies, the timing of the assessment and definitions of trauma. Estimates of psychological symptoms following musculoskeletal trauma have ranged from 6.5% to 51.0%. Mason assessed the psychological state of 210 male accident and emergency department patients and followed them for 18 months, at which time 30% satisfied criteria for a psychiatric disorder. A recent study of patients with severe lower limb injuries found a 42% prevalence of psychological disorder at 24-month follow-up and that only 22% of such patients reported receiving mental health services. No relation was found between injury severity and psychological distress; however, the authors suggested that low variability in injury severity might have obscured this result. McCarthy further identified a high correlation between the Brief Symptom Inventory (a measure of psychological distress) and the Sickness Impact Profile (a measure of patient function). A high index of suspicion for the presence of psychiatric disorders is important in treating the orthopaedic patient with multiple trauma, chronic disease, factitious disorder, or suspected malingering or who fails to improve with recognized treatment. Recognition of a psychiatric problem should be part of preoperative planning in orthopaedic practice, and a formal psychiatric referral for diagnosis and treatment should be made for the patient with significant psychiatric involvement. When associated psychiatric disease is diagnosed and controlled before orthopaedic treatment commences, the patient is more likely to comply with the treatment regimen, which may lead to better results. It is important for providers who care for patients with minor injury to include a psychiatric history and/or rapid screening for psychiatric disorders as part of the health assessment. Psychosocial factors, specifically, ongoing litigation and psychological symptoms are related with reduced health-related quality of life. Further, the goal of care is to help patients attain maximal functional recovery. Therefore, the presence of a positive psychiatric history or a current psychiatric disorder should stimulate a referral of these patients for appropriate emotional support and therapeutic follow-up. By doing so, providers will give patients important interventions to maximize full recovery.
Abstract: Little is known about the clinical consequences of psychological morbidity associated with orthopedic trauma. Previous work has reported that mental illness is an independent predictor of poor outcome following orthopedic trauma, and future studies should explore whether management of psychological symptoms independently predicts recovery from orth...
Show More
-

Acute Psychotic Episode in Psychostimulant Drug Addicted Teenager
Lavinia Alexandra Moroianu,
Alexandru Bogdan Ciubară,
Anamaria Ciubară,
Aurel Nechita
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
23-23
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.33
Downloads:
Views:
Abstract: Background: Consumption of psychostimulant drugs is a medical problem of the entire world because of the growing number of consumers, while developing global drug trafficking. The predisposition for psychostimulant drugs is primarily influenced by the psychological structure of the individual (persons instability, histrionic personality, anxious type), the individual's age, but also depending on social, environmental, family, professional factors. Prevalence of drug use is highest in the age group between 16-30 years when teenagers are prone to increased vulnerability, especially those with serious emotional problems.
Aims:To emphasize the importance of recording and following the intellectual, emotional and social development of the addictive teenagers after a psychotic episode induced by drugs consumption and adapting treatment for each of these pacients.
Methods: Use of psychostimulant drugs can cause symptoms of psychosis. People who are addicted to psychostimulant drugs can experience psychotic symptoms. Approaching this pathology in terms of a clinical case aims to highlight the symptoms of an acute psychotic episode, its origin, the correct diagnosis, early treatment and evolution of a teenager patient with such an addiction. The intensity of the symptoms depends on the type of the psychostimulant drug, the timing and duration of consumption, and the dosage. In many cases, people only need to take antipsychotics for a short time to get their symptoms under control. People with schizophrenia may have to stay on medications for life.
Results and Discussions: It is also very important to recognize an acute psychotic episode and administer an early treatment which can change the course of a potentially illness. It is required a fast and adequate medical intervention established by a multidisciplinary team formed by a psychiatrist, a psychologist and a medical assistant who can help stopping the consumption of psychostimulant drugs, for following up the evolution of the patient, the acceptance of the treatment and also for social reinsertion.
Conclusion: In Romania, it is compulsory to understand the necessity of a multidisciplinary team to work together for the wellbeing of a patient, for the family and friends of the patients to recognize and to admit the modifications in someone’s behavior and the administration of adequate medication in early stages of an illness to change its` course or to stop its’ evolution.
Abstract: Background: Consumption of psychostimulant drugs is a medical problem of the entire world because of the growing number of consumers, while developing global drug trafficking. The predisposition for psychostimulant drugs is primarily influenced by the psychological structure of the individual (persons instability, histrionic personality, anxious ty...
Show More
-

Alcohol Consumption – Implications in Orthopedic Trauma
Andrei Bradeanu,
Razvan Tudor,
Paul Dan Sîrbu,
Anamaria Ciubară,
Loredana Pascu,
Alexandru Bogdan Ciubară
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
24-24
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.34
Downloads:
Views:
Abstract: In mental health field is established that alcohol consumption can exacerbate an underlying mental health disorder. Among people with severe mental health are common alcohol problems. Alcohol depress the central nervous system and this might produce moods fluctuation and worsen the depression and anxiety. At heavy and/or chronic drinkers were reported several symptoms involving cognitive ability including diminished brain size, memory loss, loss of attention span, loss of visuospatial abilities, inability to think abstractly, Wernicke-Korsakoff syndrome. Alcohol can temporarily alleviate feelings of depression and anxiety, so people tend to use it as a form of ‘self medication’ in order to cheer themselves up or as a sleep help. But also, alcohol can disturb the body’s ability to rest, so it can lead to reduced energy levels. The key to mental health patients who regularly consume alcohol is the toxic cyclical process created. At first, one drink to relieve depression, but alcohol deplete serotonin levels, so the patient feels more depressed and thus necessitating more alcohol to ‘treat’ his depression. Sometimes it can also reveal or intensify underlying feelings, evoke past memories of trauma or any other event associated with painful feelings. Moreover, alcohol has pain-reducing properties (sustained also in a systematic review published in December 2016 issue of “The Journal of Pain”) by decreasing the activity of nerves within the brain. Furthermore, this chronic ‘self medication’ with alcohol has a wider action on the body.
1. Growing Bone - Epidemiological studies shows that chronic alcohol consumption at young age affect the bone’s health; it has multiple effects on osteoblasts (forming cells), slows down the bone turnover and can increase the risk of osteoporosis.
2. Adult Bone - There were studies on animals and researches in human adults made to prove the relationship between alcohol consumption and bones’ health. The results show that the alcohol consumption is less damaging for adults than young people, but research has shown that seventh decade women or older who consumed an average of more than 3 ounces of alcohol/day (equivalent of six drinks) had greater bone loss than women who had minimal alcohol intake. (Hannan et al. 2000) So postmenopausal chronic heavy drink women have an increased risk of osteoporosis and bone fractures. Researches suggest that alcohol consumption and poor nutrition and/or tobacco use lowers even more bones’ mineralization and increase the likelihood of bone fractures. Dr. Iliriana Bisha Tagani presented for SteadyHealth the relationship between alcohol consumption and joint pain. Alcohol dehydratate the organism because of it’s diuretic properties. Ligaments are structures rich in water and need water periodically to remain soft and spongy. So high alcohol consumption leads to excess removal of water from the body. The ligaments are one of the first to get affected by dehydration so they lose from their elasticity and any movement of the joints can lead to unbearable pain and arthritis (moreover, alcohol is considered an arthritis „trigger food”).
3. Immunity - Chronic heavy consumption of alcohol can suppress the immune system after a period of time. It can also cause neuropathy, making someone feel a pins and needles sensation in their extremities, a compounded effect with those who suffer from arthritis.
In conclusion, patients with mental health disorder present an increase tendency of alcohol abuse, which predominant leads to articular and bones disfunctions. These patients also presents a high tolerance pain due to analgestic and neuropathic effects which frequently masks the symptoms of affections like arthritis.
Abstract: In mental health field is established that alcohol consumption can exacerbate an underlying mental health disorder. Among people with severe mental health are common alcohol problems. Alcohol depress the central nervous system and this might produce moods fluctuation and worsen the depression and anxiety. At heavy and/or chronic drinkers were repor...
Show More
-

Psychiatric Comorbidities in Oncological Patients
Diana Stanculescu,
Adelina Dubas,
Ruxandra Slavu,
Romulus Hagiu,
Mihai Bran
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
25-25
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.35
Downloads:
Views:
Abstract: Introduction: Oncological patients have many psychiatric comorbidities. Whatever the therapy, the burden of the immediate, long term and late effects of these treatments adds to the inherent distress.
Aims: The objective of the study was to assess the psychiatric comorbidities and the quality of life of oncological patients receiving chemotherapy and radiotherapy.
Methods: 65 patients with different localization tumors were included in this observational study. Some receiving chemotherapy, some radiotherapy and some both. All patients were assessed using the Hospital Anxiety and Depression Scale (HADS) for anxiety and depressive symptoms, Montreal Cognitive Assessment (MOCA) for cognitive impairment and Quality of Life Enjoyment and Satisfaction Questionnaire – Short Form (Q-LES-Q-SF) for the quality of life before the oncological treatment and after one or three months of treatment. Patients with diagnosis criteria for depression or anxiety disorders received the recommended psychotropic treatment.
Results: Patients with brain tumors receiving radiotherapy had lower scores on MOCA tests as opposed to patients receiving chemotherapy for any type of cancer that scored lower on the MOCA during their chemotherapy. Men scored more for anxiety and while women seemed more depressed but with better perspective on their outcome. The quality of life was correlated with the level of disability produced by the disease and treatment. 23 patients received antidepressant treatment during the study for depressive symptoms or anxiety. Patients receiving antidepressants showed better scores on HADS, MOCA and Q-LES-Q-SF scales.
Conclusions: Psychiatric comorbidities are very frequent among oncological patients and can affect their quality of life. Antidepressant use among these patients could be neuroprotective and could improve their quality of life.
Abstract: Introduction: Oncological patients have many psychiatric comorbidities. Whatever the therapy, the burden of the immediate, long term and late effects of these treatments adds to the inherent distress.
Aims: The objective of the study was to assess the psychiatric comorbidities and the quality of life of oncological patients receiving chemotherapy an...
Show More
-

Fractals in Our Mind: Chaos Theory in Psychiatry
Ocrain P. Radu,
Curt C. Alina-Isabela,
Dobrin L. Andra-Ioana
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
26-26
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.36
Downloads:
Views:
Abstract: Background: From a mathematical perspective, dynamics can be thought of as linear or non-linear. Linear equations work quite well for a number of problems in the physical sciences. For instance, they are very useful if one wants to predict the orbit of the planets or understand the effects of wind resistance and gravity on the trajectory of a missile. To explore systemic change, non-linear dynamics uses non-linear equations. Non-linear equations are not additive; therefore, they are often difficult to solve. Non-linear systems tend to settle down over time. This settling down, or convergence, tends to result in one of four typical patterns. These patterns, when graphed in diagrams that show periodic changes in behaviour, are called attractors. The trajectories of these attractors typically converge on a discrete point, a simple oscillating cycle, a quasiperiodic cycle, or chaotic cycle. A practical translation of this is the fractal, an object consisting of a pattern that when magnified, reveals repetitive levels of detail so that a similar structure exists on all scales. This property is known as self-similarity.
Aims: To examine a novel view-point by examining the possible applications of chaos theory in the study of mental health. Method: For this paper, we studied the available research correlating chaos theory and mental health, especially schizophrenia and bipolar disorder.
Results and Discussion: The papers we reviewed show dynamic and chaotic models for both schizophrenia and bipolar disorder. Examples have been found of chaotic responses to initial stimuli in schizophrenia where overstimulation or sensory overload may be paradoxically associated with negative symptoms, fixity, or even catatonia. Meanwhile, regarding bipolar disorder, the attractor hypothesis has been analysed. It is thought that healthy persons have a single strange attractor regarding their mood shifts, while in patients suffering from bipolar disorder, this attractor is destroyed and replaced by two attractors with chaotic transients between them. The second pillar of chaos theory has also been analysed regarding mental health by using fractal analysis to more accurately determine MRI changes in mental patients.
Conclusion: This analysis is still in the opening phases and more research is needed to further cement chaos theory as a valid approach in psychiatry, especially since initial results seem promising.
Abstract: Background: From a mathematical perspective, dynamics can be thought of as linear or non-linear. Linear equations work quite well for a number of problems in the physical sciences. For instance, they are very useful if one wants to predict the orbit of the planets or understand the effects of wind resistance and gravity on the trajectory of a missi...
Show More
-

Family Support of Children with Politrauma and Severe Trauma
Eva Maria Cojocaru,
Roxana Elena Bogdan Goroftei
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
27-27
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.37
Downloads:
Views:
Abstract: Introduction: Children are often presenting in the emergency room with mild to severe politrauma. This requires rapid and firm actions which can be perceived as brutal by the families. The child will be sourrounded by many equipments, spccial measures must be taken to maintain vital functions and to prevent infection so in many cases parents are invited to step out of the room where the life-saving maneuvers and treatments are done. Frustration, guilt, anxiety, grief and uncertainty are felt by the parents. On the other hand health professionals defy actions under great pressure, uncertainity, sometimes disfunctionality betewwen the saving team members or tehnical difficulties due to wasteor inadequate equipments.
Methods: We want to present cases of politraumatised children, acute intervention in the emergency room of the health professionals,and after the overcome of the dramatic moments of the life-saving actions the long term surveillance of the children and their families. Politrauma is due often to car, motor or bike accidents, as also sometimes of suicidal actions of the children. Even if the accident is incidental and is pure randomly family guilt always exist and is hard to overpass. In many situations parents have delegated the surveillance of the child to other children of the family or other relatives (uncles, cousins, grandparents) and then discussions and throwing guilt appear.
Reesults: And discussion: In the presented cases the politraumatised children had all a very good evolution. All the children were treated in our hospitals form Galati and underwent, anticonvulsivant therapy, intubation and care in the intensive care unit, as also surgical interventions (for bone fractures or other) and all steps were done with the accompaniment of the psychologist of our clinic.
Conflict of interest disclosure: the authors have no conflict of interest and this research has not a financial support for the authors.
Abstract: Introduction: Children are often presenting in the emergency room with mild to severe politrauma. This requires rapid and firm actions which can be perceived as brutal by the families. The child will be sourrounded by many equipments, spccial measures must be taken to maintain vital functions and to prevent infection so in many cases parents are in...
Show More
-

Psychiatry and Family Medicine – What General Practitioners from Galați County Think
Alina M. Pleșea-Condratovici,
Cristian-Marius I. Găinaru,
Cătălin I. Pleșea-Condratovici
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
28-28
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.38
Downloads:
Views:
Abstract: Background: Traditionally considered the base of medical care, first contact with patients and their family and the gatekeeper of the medical system, family medicine of nowadays is trying to survive underfunding, exhaustion and bureaucracy. The impact of the current situation on the psychiatric patients is profound, meaning prolonged wait time to see a specialist and costly diagnostic errors.
Aims: To identify major system flaws related to psychiatric area from the GP’s point of view in order to propose the best course of action for an increased quality of psychiatric case management in primary care.
Method: An online questionnaire was completed by 41 out of 244 general practitioners from Galati County, Romania. The questionnaire investigates the main hurdles encountered by the GP in relation with the psychiatric patient, originated from the lack of adequate health policies on the one side, and the lack of patient education on the other side.
Results and Discussion: Compared to other pathologies, psychiatric diseases seem to be underdiagnosed and undertreated. There is an acute need for psychiatric medical training - only 7% of responders attended courses in psychiatry in the last 5 years despite the fact that 97.7% think that a psychiatry course or manual oriented to family doctors is needed. Communication training is needed too, 88.4% of doctors report difficulties in persuading patients to present themselves at psychiatric services. 81.4% of doctors initiate psychotropic medication on a “sic volo” basis, in the absence of any prescription protocols. A systematic use of psychiatric scales is a necessity - only one doctor out of 41 uses psychiatric scales although 97.7% of participants agree to use them, preferably integrated in the medical software and paid.
Conclusion: Two main interventions are to be performed: specific medical training in the psychiatric area adapted to GP’s needs, including communication skills, GP adapted psychiatric scales and manuals and reconsideration of subsidized medicines policy for psychiatric drugs.
Abstract: Background: Traditionally considered the base of medical care, first contact with patients and their family and the gatekeeper of the medical system, family medicine of nowadays is trying to survive underfunding, exhaustion and bureaucracy. The impact of the current situation on the psychiatric patients is profound, meaning prolonged wait time to s...
Show More
-

Rehabilitation after Hip Fracture Surgery in Dementia and Cognitively Intact Patients
Alexandru Bogdan Ciubară,
Paul Dan Sîrbu,
Razvan Tudor,
Viorel Oltenacu,
Roxana-Cristina Damaschin,
Anamaria Ciubară
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
29-29
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.39
Downloads:
Views:
Abstract: Introduction. The combined presentation of dementia and hip fracture in the elderly is emerging as a significant health issue worldwide. An individual with dementia is up to 3 times more likely than a cognitively intact older adult to sustain a hip fracture.
Objectives. 10 participants were recruited, 7 were women and 3 were cognitively impaired. Mean age was 80 years. All hip fractures are treated with surgery. This study analyzes recovery, incidence of delirium and 30-day mortality, after hip surgery.
Results and discussion. Patients with dementia make poor functional recoveries after hip fracture as compared to nondemented patients. Individuals with dementia use rehabilitation less after hip fracture surgery. Early operative intervention is important to patients because it results in less pain, which in turn leads to lower incidence of delirium. Patients with dementia experience higher rates of all-round morbidity and mortality following hip fracture.
Conclusion. The goal of acute-care hospital treatment of patients with hip fractures including those with dementia is to achieve the following outcomes: short time to surgery, few or no complications, control of pain, and early mobilization for restoration of function and gait. Following a hip fracture, patients with dementia are at higher risk of mortality and functional decline than those who are cognitively intact.
Abstract: Introduction. The combined presentation of dementia and hip fracture in the elderly is emerging as a significant health issue worldwide. An individual with dementia is up to 3 times more likely than a cognitively intact older adult to sustain a hip fracture.
Objectives. 10 participants were recruited, 7 were women and 3 were cognitively impaired. Me...
Show More
-

Postfracture Rehabilitation after Hip Fracture in Patients with Dementia
Alexandru Bogdan Ciubară,
Sorin Ungurianu,
Razvan Tudor,
Viorel Oltenacu,
Roxana-Cristina Damaschin,
Anamaria Ciubară
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
30-30
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.40
Downloads:
Views:
Abstract: Introduction. Hip fractures are more common especially in women, in the elderly, due to osteoporosis. Almost half of all people who suffer hip fractures also have dementia. Patients with dementia recover slower and they are more prone to complications.
Objectives. We present 6 female patients (65 years and older) with dementia who received a different therapy: 3 surgical and the other 3 who were unfit for surgeries were treated conservatively. The main reason for non-operative intervention was the latter stages of dementia, consistent with an anticipated rapid deterioration or death.
Results and discussion. In conservative treatment group, no female could walk with assist or independently compared with surgical grop where 1 female could walk with assist. Conservative group had less desire for active treatments and rehabilitation. At long-term quality of life in the surgical group was not higher than reported following conservative care group.
Conclusion. There is insufficient evidence to draw conclusions about how effective is the surgical treatment or non-surgical care for people with dementia and hip fracture. Increased attention should be focused on efforts to enhance comfort in this patient population.
Abstract: Introduction. Hip fractures are more common especially in women, in the elderly, due to osteoporosis. Almost half of all people who suffer hip fractures also have dementia. Patients with dementia recover slower and they are more prone to complications.
Objectives. We present 6 female patients (65 years and older) with dementia who received a differe...
Show More
-

Strategies to Prevent Delirium in ICU
Mary-Nicoleta Lupu,
Mădălina-Nina Sandu
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
31-31
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.41
Downloads:
Views:
Abstract: Introduction: In the recent years there has been an increase in the use of psychoactive drugs, especially in adolescents and young people. Known as the "ethnobotanics", they are synthetic drugs produced in clandestine locations. Traded under different names - dried plants, scented sticks, bath salts, etc., they can induce states of euphoria, lack of fatigue, low appetite, amnesia, detachment. The undesirable effects consist of hallucinations, panic attacks, paranoia, aggressive behavior, and in the event of an overdose there are nausea, vomiting, hemodynamic instability, tachycardic pulse, seizure risk, coma.
Material and method: Four young patients were admitted in the Intensive Care Unit with a very serious general condition, deeply comorbid, following the ethnobotanic consumption. The treatment consisted of hydroelectrolytic rebalancing, vital function support, mechanical ventilation.
Results and Discussion: Under specific therapy for intensive care and careful monitoring of vital functions, evolution was favorable, allowing patients to be transferred to the department and subsequently taken over by the psychiatrist to assess drug addiction and specific treatment.
Conclusions: The lack of information on the chemical composition has hampered the therapy of these patients, this being especially oriented towards the treatment of dysfunctions and organ failure.
Abstract: Introduction: In the recent years there has been an increase in the use of psychoactive drugs, especially in adolescents and young people. Known as the "ethnobotanics", they are synthetic drugs produced in clandestine locations. Traded under different names - dried plants, scented sticks, bath salts, etc., they can induce states of euphoria, lack o...
Show More
-

Managing the Fractures Treatment for Patients Who Develop Alchohol Withdrawal
Sorin Ungurianu,
Florentin Dimofte
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
32-32
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.42
Downloads:
Views:
Abstract: Aims: Southern Moldova is a wine region, with a lot of wineyards. Every peasant has in his farm some wine aryl’s and produces annual hundreds liters of wine and brandy which he consumes daily. In this area the water is not drinkable, is used just for washing. At least 2 patients from the total that are hospitalized in a week, are having alcoholic whitdrawal.
Material and Methods: this work is an epidemiological study on a 5 years period between 2012-2016 on a cohort of 485 patients that were hospitalized and received surgical intervention for different tipes of fractures in the Orthopedics and Trauma Department of Clinic Emergency Hospital “Sf. Andrew” Galati. Those patients had an alcoholic withdrawal by the time they were hospitalized. 67 of them were transferred to the psychiatry department to receive special treatment, 365 continued the treatment in our department and 53 of them received during the hospitalization variable quantities of alcohol to avoid alcohol withdrawal. From all 485 patients, 208 patients had superior limb fractures and the rest of 277 patients had an inferior limb fractures. Complications occurred only in patients with an inferior limb fractures (67) because of the personality disorders and alcoholic dementia, they didn’t respect the indications received.
Results and Discussion: Alcoholic withdrawal started usually after 48 hours from hospitalization. From the 67 patients that were transferred to the psychiatry department, in 23 of them could receive the surgical intervention in the first days, and the rest after returning from the psychiatry department. In all the patients that had surgical intervention before de alcoholic withdrawal, we tried external fixation also with casts for surgical safety. 11 of them returned with fracture and osteosynthesis materials displaced and therefore another surgical intervention. The rest of 44 patients that didn’t received surgical intervention and transferred to the psychiatry department, 24 of them had complications like from an undisplaced fracture they transformed into a displaced one, 2 of them had compartment syndrome, 4 of them profund venous thrombosis, 11 bleeding blisters, 2 transformed a closed fracture into a open fracture and 4 of them pulmonary embolism.
From all 365 that had treatment In our department, 8 of them had bleeding blisters, 6 profund venous thrombosis, 5 compartment syndrome, 4 pulmonary embolism and 7 transformed the closed fracture into an open one. The 53 patients that received small doses of alcohol neighter one of them had any postoperatively complications.
Conclusions: every patient that could develop alcoholic withdrawal during the hospitalization, must be diagnosed from the beginning and treated by sustaining his metabolism, vitaminotherapy and hipnotics or they could get an alcoholic treatment to avoid withdrawal?
Abstract: Aims: Southern Moldova is a wine region, with a lot of wineyards. Every peasant has in his farm some wine aryl’s and produces annual hundreds liters of wine and brandy which he consumes daily. In this area the water is not drinkable, is used just for washing. At least 2 patients from the total that are hospitalized in a week, are having alcoholic w...
Show More
-

Therapeutic Management in Resistant Depression
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
33-33
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.43
Downloads:
Views:
Abstract: Background: Depression is a major public health problem. Resistant depression occupying a growing share in psychiatric pathologies.
Aim: To identify the effectiveness of strategies to overcome resistant depression.
Methods. To determine the clinical outcome in patients with resistant depression was planned a descriptive cohort study on a group of 612 patients.
Results and Discussion. Subjects with resistant depression are a major therapeutic challenge for mental health experts. Assessing risk factors for treatment-resistant depression is equally important to guide mental health professionals on an appropriate management plan. In the treatment of these patients have taken a comprehensive attitude to the needs of patients, their individual ways of social functioning. These attitudes have allowed overcoming fears patient and his family on misconceptions about the disease and stigmatization. Since polymorphic psychopathology induced difficulties in choosing treatment, the multitude of symptoms was grouped into several major clinical syndromes. Therapeutic management was based on increasing the dose, strategies of switching, combining and augmentation.
Conclusion: The use of historical, clinical, psychological, analytical epidemiology, descriptive epidemiology, and mathematical methods, but also the calculation of RR (relative risk), CI (confidence interval), χ2, NNT (number needed to treat patients) and other indices indicated that the most significant reduction was observed in basal symptoms of patients: depressed mood, psychomotor slowness, weight loss, sleep disturbed.
Abstract: Background: Depression is a major public health problem. Resistant depression occupying a growing share in psychiatric pathologies.
Aim: To identify the effectiveness of strategies to overcome resistant depression.
Methods. To determine the clinical outcome in patients with resistant depression was planned a descriptive cohort study on a group of 612...
Show More
-

The Effect of Psychoeducation and Anxiety Therapy in Breast Cancer Screening
Livia Teodora Lungulescu,
Cristian Virgil Lungulescu,
Victor Gheorman,
Sorin Nicolae Dinescu,
Veronica Calborean,
Mihail Cristian Pîrlog
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
34-34
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.44
Downloads:
Views:
Abstract: Background: Depressive symptoms are commonly found in patients diagnosed with mammary cancer. The association between symptoms of depression and anxiety could exacerbate the subjective symptoms of the oncological disease, worsening both the evolution of the illness and the response to treatment. Previous studies proved that the psycho-education applied on oncological patients had good results over anxiety and depression, but also over symptoms like pain or nausea.
Aims: Our research was focused to evaluate the effect of psycho-education over the anxiety of the women prone to face screening mammography.
Method: Our study was conducted at the Emergency Clinical County Hospital Craiova, Romania and involved 50 subjects divided in two groups:
a. Group A of 25 patients, who benefited of psycho-education before mammography. The screening of the anxiety symptoms was realised using STAI test, before and after mammography.
b. Group B with the same number of subjects evaluated by mammography and STAI test without psycho-education.
Results and Discussion: In the group A, the anxiety symptoms were correlated with aging. The psycho-educational intervention had an anxiolytic effect statistically significant in patients between 40 and 49 years old (p<0,05).
Conclusion: These data suggests the necessity of the psycho-educative intervention in order to decrease the level of anxiety of the target population for breast cancer screening–and making them more likely to participate in other screening activities; anxiety increased also by many clinical and paraclinical interventions. In that way, it would be useful to develop new research to see the effects of psychoeducational interventions also in other medical departments.
Abstract: Background: Depressive symptoms are commonly found in patients diagnosed with mammary cancer. The association between symptoms of depression and anxiety could exacerbate the subjective symptoms of the oncological disease, worsening both the evolution of the illness and the response to treatment. Previous studies proved that the psycho-education app...
Show More
-

Title: Overlap of Attention Deficit and Hyperreactivity Disorder with Obstructive Sleep Apnea – A Case Presentation
Carmen Columbia Stroescu,
Stefan Dumitrache-Rujinski,
Vlad Bogdan Stroescu,
Ionela Erhan,
Alina Croitoru,
Miron Alexandru Bogdan
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
35-35
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.45
Downloads:
Views:
Abstract: Introduction: Obstructive sleep apnea (OSA) is more prevalent in psychiatric patients than in general population. Early diagnosis and adequate management of OSA could improve prognosis in this category.
Methods: We present a case of moderate OSA in a patient with attention deficit and hyperreactivity disorder (ADHD) with prominent symptoms following a H1N1 viral encephalitis.
Results and discussion: 31 years-old male, night shift-worker, active smoker, overweight, on long-term psychotropic therapy (extended release methylphenidate), with partial response to therapy. Reports frequent arousals, sometimes feeling like gasping or choking, unrefreshing sleep, chronic fatigue. Epworth Sleepiness Scale score was 10/24 (excessive daytime sleepiness). STOP-Bang Questionnaire score was 3/8 (high risk of OSA). Home unattended cardio-respiratory poligraphy identified moderate OSA and Positive Airway Pressure (PAP) therapy was prescribed. At 1 year follow-up: works during daytime, improved performance with lower dose of stimulant medication; agrees to adhere to a smoking cessation programme; no weight loss.
OSA could be responsible for both night time and daytime symptoms in psychiatric patients. The STOP-Bang Questionnaire (a screening tool for OSA) identifies subjects at risk for this condition.
PAP therapy improved the patient’s performance and also allowed lowering of psychotropic medication dose.
Research support: No conflict of interest to disclose.
Abstract: Introduction: Obstructive sleep apnea (OSA) is more prevalent in psychiatric patients than in general population. Early diagnosis and adequate management of OSA could improve prognosis in this category.
Methods: We present a case of moderate OSA in a patient with attention deficit and hyperreactivity disorder (ADHD) with prominent symptoms following...
Show More
-

Comorbidity of Depressive Symptomatology in Patients Aged 60-80 Years with More than Two Chronic Physical Illnesses in General Practice
Ivo Natsov,
Rumen Triffonov,
Svetlana Velikova,
Vladimir Nankov,
Kaloian Natsov
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
36-36
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.46
Downloads:
Views:
Abstract: Objectives: To investigate the prevalence of clinically relevant and subsyndromal depressive symptoms in patients aged 60-80 years with more than two somatic diseases; To approbate PRIME-MD as a tool for investigating depression in later life; to verify the hypothesis that the presence of more than two somatic diseases is a predictor of depression.
Method: from October 2014 to March 2016 the group of patients in the age 60-80 years with more than two documented chronic diseases were investigated by means of PRIME-MD. The assessment of multimorbidity was done using the patients health records. Its burden was assessed by the Cumulative Illness Rating Scale.
Results: depressive syndromes were significantly more frequent in patients with multimorbidity. Multimorbidity is associated with a higher sum of points in PHQ- 9 and heavier levels of depressive symptoms in comparison with the general population. PHQ- 9 is a fast and reliable tool for evaluating depression in later life.
Conclusion: multimorbidity is the rule rather than exception in later life. Diagnosis of depression in patients with multimorbidity may be difficult because of the manifestation of depressive symptoms as somatic. Probably there is a need of mandatory screening for depression in patients with more than two chronic physical disorders in general practice.
Abstract: Objectives: To investigate the prevalence of clinically relevant and subsyndromal depressive symptoms in patients aged 60-80 years with more than two somatic diseases; To approbate PRIME-MD as a tool for investigating depression in later life; to verify the hypothesis that the presence of more than two somatic diseases is a predictor of depression....
Show More
-

Objective Quantification of Psychomotor Disturbances in Patients with Depressive Episode
Svetlozar H. Haralanov,
Petya D. Terziivanova,
Evelina S. Haralanova
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
37-37
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.47
Downloads:
Views:
Abstract: Background: Psychomotor disturbances have been regarded as cardinal symptoms of depression for centuries and their objective assessment may have predictive value with respect to the severity of clinical depression, treatment outcome and prognosis of the depressive disorder. In clinical practice psychomotor disturbances are evaluated and measured subjectively – by clinical observation and/or by rating scales.
Aims: To introduce a novel objective approach for recording and measuring psychomotor activity and reactivity in patients with clinical depression.
Method: Psychomotor indicators of activity and reactivity were objectively recorded and measured by computerized ultrasonographic cranio-corpo-graphy.
Results and Discussion: Objective and quantitative assessment of psychomotor symptoms may have pathophysiological significance as psychomotor disturbances go along with affective dysregulation. It is supposed that common neurotransmitter pathology in the brain structures causes simultaneously psychomotor and affective dysregulation that underlies the pathophysiology of depressive disorder. Also, psychomotor retardation is thought to be a cardinal depressive symptom in endogenous depressions – unipolar and bipolar. On the other hand, psychomotor agitation may be considered as latent bipolarity, although the presence of manic symptoms within a depressive state and the role of psychomotor agitation in depressive patients are still disputable.
Conclusion: Integration between different methods is needed in order to improve the understanding of psychopathology and neurobiology of a disputable diagnosis such as clinical depression. We introduce in the field of psychiatry an objective and quantitative approach, which could permit psychomotor discrimination not only between depressive patients and healthy controls, but also between subgroups of depressive patients.
Abstract: Background: Psychomotor disturbances have been regarded as cardinal symptoms of depression for centuries and their objective assessment may have predictive value with respect to the severity of clinical depression, treatment outcome and prognosis of the depressive disorder. In clinical practice psychomotor disturbances are evaluated and measured su...
Show More
-

Kaplan Meiers Method in Comparison and Randomised Clinical Trials of Valproate Versus Lithium and Carbamazepine in Treatment of Bipolar Patients in Albania
Fatime Elezi,
Sonila Tomori,
Eugjen Sotiri,
Elizana Petrela
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
38-38
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.48
Downloads:
Views:
Abstract: Background: The Kaplan Meir procedure is a method of estimating time-to-event models in the presence of censored cases. Kaplan Meier (K-M) model is based on estimating conditional probabilities at each time point when an event occurs and taking the product limit of those probabilities to estimate the survival rate at each point in time.
Aims: Application of Kaplan Meier method to compare the efficacy of Valproate versus lithium and carbamazepine in the long-term treatment of bipolar patient.
Method: 235 patients with at least two episodes of bipolar disorders (DSM-IV) in Psychiatric service in UHC-Tirana. We have estimated age, sex, education, occupation, comorbidities, types and subtypes of bipolar disorders. This is a longitudinal, comparison and randomized clinical trial, with a duration of 2 years, three equal parallel-groups with open label pre-randomized phase. Primary outcome measure was time to relapse/recurrence to any mood episodes and Survival analyses was performed.
Results and Discussion: Long- rank test was used to test the significant difference between the survival experiences of bipolar patients. Cumulative survival for valproate’s group was 26% higher than carbamazepine’s group. While mean and median survival time were respectively 35% and 53% longer for valproate. Carbamazepine showed approximatively the same effect as valproate in some subtypes of bipolar disorders and with comorbidity.
Conclusion: Kaplan Meier is an useful method to estimate the comparison effect of Valproate versus Lithium and carbamazepine. Valproate is significantly more effective than lithium and carbamazepine in prophylactic treatment of bipolar disorders.
Abstract: Background: The Kaplan Meir procedure is a method of estimating time-to-event models in the presence of censored cases. Kaplan Meier (K-M) model is based on estimating conditional probabilities at each time point when an event occurs and taking the product limit of those probabilities to estimate the survival rate at each point in time.
Aims: Applic...
Show More
-

Treatment Alternatives in Resistant Obsessive-Compulsive Disorder in Children – A Review of the Last Five Years Literature
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
39-39
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.49
Downloads:
Views:
Abstract: Background: Obsessive-compulsive disorder (OCD) in childhood and adolescence is an impairing condition, associated with a specific set of distressing symptoms.
Aims: To review the last five years research according the treatment of treatment-refractory paediatric obsessive-compulsive disorder (OCD).
Method: A PubMed search was conducted to identify the last five years controlled trials in paediatric OCD in order to identify the possible treatment alternatives.
Results and Discussion: Pharmacotherapy with selective serotonin reuptake inhibitors (SSRIs) and cognitive-behavioural therapy are effective treatments for paediatric OCD. In cases of resistance the possible alternatives we provided are increasing the dose of SSRI, switching to another SSRI, augmentation with antipsychotics, and the use of serotonin nor-adrenaline (norepinephrine) reuptake inhibitors (SNRIs) and monoamine oxidase inhibitors (MAOIs) this considering pharmacological alternatives. We also found data of non-pharmacological treatment to be effective including family interventions and physical interventions such as neurosurgery and deep brain stimulation, alongside the pharmacological strategies. Roughly one-quarter to one-third of children do not experience a treatment response with first-line treatments for OCD. A large number of children with OCD judged to be “clinical responders” in treatment studies still have significant residual symptoms.
Conclusion: Several pharmacological and non-pharmacological treatment alternatives exist for children with resistant OCD symptoms but there is a very few evidence-based data on this alternatives and further researchers is needed in this field.
Abstract: Background: Obsessive-compulsive disorder (OCD) in childhood and adolescence is an impairing condition, associated with a specific set of distressing symptoms.
Aims: To review the last five years research according the treatment of treatment-refractory paediatric obsessive-compulsive disorder (OCD).
Method: A PubMed search was conducted to identify t...
Show More
-

Improving Metabolic Adverse Events Associated with Antipsychotic Treatment in Children and Adolescents
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
40-40
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.50
Downloads:
Views:
Abstract: Background: Children and adolescents with serious mental illness may experience improved psychiatric stability with second generation antipsychotic (SGA) medication treatment, but unfortunately may also experience unhealthy weight gain adverse events.
Aims: To describe behavioral weight loss intervention for weight gain children and adolescents being treated with antipsychotic medications.
Method: Six obese children and adolescents with long-term antipsychotic medication exposure were included in the study. The efficacy of the intervention was evaluated with a battery of anthropomorphic and metabolic assessments, including weight, body mass index percentile, whole body adiposity, liver fat content, fasting plasma glucose and lipid levels. Participants and their parents also filled out a treatment satisfaction questionnaire after study completion.
Results and Discussion: All participants attended all sixteen sessions of the intervention and experienced beneficial changes in adiposity, fasting lipid levels, and liver fat content associated with weight stabilization. Participants and their parents reported a high level of satisfaction with the treatment.
Conclusion: Antipsychotic-related weight gain is an important public health issue for children and adolescents requiring ongoing antipsychotic treatment to maintain psychiatric stability. Family-based behavioral weight loss treatment can be feasibly delivered and is acceptable to children and adolescents taking antipsychotic medications and their families.
Abstract: Background: Children and adolescents with serious mental illness may experience improved psychiatric stability with second generation antipsychotic (SGA) medication treatment, but unfortunately may also experience unhealthy weight gain adverse events.
Aims: To describe behavioral weight loss intervention for weight gain children and adolescents bein...
Show More
-

Effects of Deep Brain Stimulation in Anorexia Nervosa
Ela Mitro,
Besmira Zenelaj,
Valmira Kodra,
Dorina Sanxhaku,
Valbona Alikaj
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
41-41
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.51
Downloads:
Views:
Abstract: Background: Anorexia nervosa is characterized by a chronic course that is refractory to treatment in many patients and has one of the highest mortality rates of any psychiatric disorder. In this context, there is an urgent need to develop safe therapies approaches. Deep brain stimulation (DBS) has been applied to circuit-based neuropsychiatric diseases, such as Anorexia nervosa, Parkinson’s disease and major depression, with promising results.
Aims: To assess the safety of DBS to modulate the activity of limbic circuits and to examine how this might affect the clinical features of anorexia nervosa.
Method: Review of existing literature and research on the topic.
Results and Discussion: Deep brain stimulation (DBS) of the subcallosal cingulate in patients with highly treatment–resistant anorexia nervosa can significantly improve mood, anxiety, affective regulation, and body weight.
Conclusion: According to different studies, deep brain stimulation might alter the brain circuits that drive anorexia nervosa symptoms and help improve patients’ mental and physical health. While our results show some early promise, more research will be needed. Findings emphasize the need for continued research into novel neuromodulation strategies for anorexia nervosa, and for psychiatric disorders more broadly.
Abstract: Background: Anorexia nervosa is characterized by a chronic course that is refractory to treatment in many patients and has one of the highest mortality rates of any psychiatric disorder. In this context, there is an urgent need to develop safe therapies approaches. Deep brain stimulation (DBS) has been applied to circuit-based neuropsychiatric dise...
Show More
-

"Optimal Outcomes" in Autism Spectrum Disorder, Characteristics of Children Who Lost the Diagnosis of Autism
Kodra Valmira,
Zenelaj Besmira,
Mitro Ela,
Sanxhaku Dorina,
Allkoja Brikena,
Alikaj Valbona
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
42-42
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.52
Downloads:
Views:
Abstract: Objective: To review the latest researches according the Optimal Outcomes in children with ASD and Characteristics of Children Who Lost the Diagnosis of Autism.
Method: Review of two studies: Deborah Fein at Al 2013 “Optimal outcome in individuals with a history of autism” which presents strengthened evidence that some individuals diagnosed with autism as young children do in fact lose their symptoms as they age. This study is the largest to-date and experts believe that it will change the way clinicians, scientists and parents think about autism. Characteristics of Children Who Lost the Diagnosis of Autism: A Sample from Istanbul, Turkey, a descriptive study reporting the characteristics of children who lost their diagnosis of autism and explaining the educational programs that these children followed.
Results: OO and TD groups’ mean scores did not differ on socialization, communication, face recognition, or most language subscales, although three OO individuals showed below-average scores on face recognition. Early in their development, the OO group displayed milder symptoms than the HFA group in the social domain, but had equally severe difficulties with communication and repetitive behaviors. Early intervention, high IQ and the development of communicative and language skills at an early age could be the most powerful factors contributing to an optimal outcome. These results provide strong evidence in support of the possibility of ‘recovering’ from ASD and demonstrate that it is, in fact, possible to reach a level of typical functioning, while not eliminating the possibility of residual deficits in the more subtle aspects of cognition and social interaction.
Conclusion: Although possible deficits in more subtle aspects of social interaction or cognition are not ruled out, the results substantiate the possibility of optimal outcome from autism spectrum disorders.
Abstract: Objective: To review the latest researches according the Optimal Outcomes in children with ASD and Characteristics of Children Who Lost the Diagnosis of Autism.
Method: Review of two studies: Deborah Fein at Al 2013 “Optimal outcome in individuals with a history of autism” which presents strengthened evidence that some individuals diagnosed with aut...
Show More
-

The Relationship Between Perceived Stress Levels and the Working Life Quality of Community Mental Health Center Professionals
Florida Dobi,
Enilda Duro
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
43-43
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.53
Downloads:
Views:
Abstract: Background: Nowadays, autism represents more than a medical problem, its effects being reflected not only on people diagnosed with, but also in medical professionals involved in therapy, families and communities.
Aims: to identify how stress levels of community mental health center professionals affect working life performance.
Method: This is a quantitative study, 55 participants from three Community Mental Health Centers in Tirana, 23 – 60 years old, mental health professionals (Psychiatrist, Occupational Therapist, Psychologist, Social Workers, Nurses). Self-report has been used through three questionnaires Measuring Scale of Working Life Quality (WRQoL)”; Measuring Scale of Perceived Stress Levels and Social Demographic Questionnaire Data results have been processed via SPSS statistics 21.0. Participants have been previously informed and they signed the inform consent.
Results and Discussion: Quality of Life has a positive affect on working life quality with a coefficient of 0,5 and of an importance about 70%. The better the quality of life, the higher the performance and life quality at work. Distress has a negative influence on working life performance with a coefficient (-0.455) and an importance which equals (0.00). Those who are distressed show a low quality performance at work. This study concluded that there is a strong negative correlation between perceived stress levels and working life quality of community mental health centre proffesionals. The higher perceived stress levels, the lower the quality of work performance.
Conclusion: There is a strong negative correlation between perceived stress levels and working life quality. The proffesionals who percieve high stress levels perform low quality work compared to those who experience low stress levels.
Abstract: Background: Nowadays, autism represents more than a medical problem, its effects being reflected not only on people diagnosed with, but also in medical professionals involved in therapy, families and communities.
Aims: to identify how stress levels of community mental health center professionals affect working life performance.
Method: This is a quan...
Show More
-

Mental Health Profile Disorders in Care Providers of Patients with Schizophrenia
Iva Çajupi,
Ada Velo,
Ermonela Dokle,
Enilda Duro,
Florida Dobi
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
44-44
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.54
Downloads:
Views:
Abstract: Background: It is known that individuals that provide care and services to persons that suffer from chronicle diseases like dementia, schizophrenia, mental retardation, people with major motor disorders, are in added risk to make mental health disorders.
Aims: Evaluating the frequency of some psychiatric disorders in persons that provide services and care to patients with schizophrenia.
Method: 112 persons that participated in the study were living in the same house, for at least five years, with patients diagnosed with schizophrenia All patients had a medical file at Mental Health Community Center No.1 in Tirana and they had taken services at least from one care giver and one mental health professional of the M.H.C.C No 1. The caregivers were assessing with an individual, detailed, clinical interview from the local psychiatrists. Their diagnosis was made based on DSM-IV R criteria.
Results and Discussion: Out of the total of 112 care providers, the majority were patient's mother (70%), then fathers (20%) and even brothers/sisters (10%). The care givers were found to fulfil DSM-IV-R criteria for generalized anxiety disorder (11%); depressive disorder (10%) and conversion disorder (13.3%).
Conclusion: The data from this study indicate that mental health of care providers it is likely to affect the outcome of their relatives suffering from schizophrenia. It is crucial to offer support and assistance to this target group by mental health community centers.
Abstract: Background: It is known that individuals that provide care and services to persons that suffer from chronicle diseases like dementia, schizophrenia, mental retardation, people with major motor disorders, are in added risk to make mental health disorders.
Aims: Evaluating the frequency of some psychiatric disorders in persons that provide services an...
Show More
-

Cognitive Control Therapy with ADD Children and Adolescents
Efigena Kabili,
Elona Gjoni,
Fjorind Bara,
Leidon Çadri,
Florida Dobi,
Sonila Tomori
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
45-45
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.55
Downloads:
Views:
Abstract: Background: In the whole spectrum of mental health disorders, cognitive structures play one of the most important role, both for the evolution of the disease, and also for the development of the person affected. In this context, it becomes very important to do a correct assessment of the cognitive function, and, also to preserve as much as possible the integrity of the cerebral structure involved in this process.
Aims: Emphasizing the importance of cognition and cognitive structures in ADD. Psychological intervention as a core intervention besides medical treatment.
Method: This is a theoretical study, conducted by observing and comparing data collected from the therapeutic intervention in 9 children and adolescent diagnosed with ADD and being enrolled in psychological therapy at the CMHC No.1 in Tirana in a 6 months period. The subjects underwent various evaluation sessions by psychiatrists, psychologist, speech therapist and psychomotor specialist; WISC 3R was used as the intelligence assessment scale in order to sort out mental retardation; parents not structured questionnaire was conducted at the beginning and at the end of the study. Cognitive Control Therapy was chosen as an innovative psychotherapeutic intervention to help the subject due to the need to rehabilitate these cognitive structures, to produce and coordinate the information.
Results and Discussion: It was observed an improvement in the executive functions, reduction of behavioural problems, and facilitation of attention deficit during cognitive tasks; increased pleasure during academic process.
Conclusion: Children becomes able to develop new and improved cognitive structures, gains abilities to better use thought process during studying and adaptation due to the training and awareness of their personal ways of learning and adaptation. They reveal the unconscious cognitive manoeuvres which produce sadness, laziness, anxiety and anger and learns also, to use new and appropriate mechanisms and behavioural models by emphasizing so the importance of psychological intervention in ADD.
Abstract: Background: In the whole spectrum of mental health disorders, cognitive structures play one of the most important role, both for the evolution of the disease, and also for the development of the person affected. In this context, it becomes very important to do a correct assessment of the cognitive function, and, also to preserve as much as possible...
Show More
-

The Depression of Mothers and the Impact on Children
Elona Gjoni,
Zamira Dega,
Efigena Kabili,
Florida Dobi
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
46-46
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.56
Downloads:
Views:
Abstract: Background: Maternal depression in all its forms (before and during pregnancy, post-partum, late life etc.) plays an important role in the life of the women affected, but also in the life of their children, representing an important risk factor for their mental health development.
Aims: To highlight the role of the nurse in the early identification of the mother depression impact to children; to define the mother depression impact to children.
Method: For a period of 4 weeks the nurses were trained to deal with mental health issues by mental health community staff. In study participated 24 women diagnosed with depression, 24 other women as a control group, which had children 3-5 years old, and who lives in the urban zone. Mothers and their children were observed by the nurse in their homes for about two hours twice a month. Children identified to have difficulties were sent for further evaluation to child and adolescent psychiatrists of community mental health center. Diagnoses were made based on SDM-IV-R criteria. The data were processed using SPSS statistics 21.0, using the Hi test. Significant values considered p≤ 0.05.
Results and Discussion: 54.2% children of mothers suffering from depression pose eating disorders, significant (value p˂0.05); 14.2% of control group mothers pose eating disorders (value p˂0.05); significant relational problems were found (value p˂0,05) in 8 children (33.3%) of the depressed mothers and only in 1 child (7.1%) of control group mothers. Insufficient attention with hyperactivity found so significant (value p˂0,05) 7 children (29.1%) of the depressed mothers and any children of control group mothers. No statistical significance was found for sleep problems, mood disorders, language and communication problems.
Conclusion: Depressed mothers have less interaction with their children than control mothers, show high level of anxiety compared to children of mothers who do not suffer from depression. However, there is a wide variation in the quality of interaction within the mother- child depressive mothers group.
Abstract: Background: Maternal depression in all its forms (before and during pregnancy, post-partum, late life etc.) plays an important role in the life of the women affected, but also in the life of their children, representing an important risk factor for their mental health development.
Aims: To highlight the role of the nurse in the early identification ...
Show More
-

Psychiatric Comorbidity in Adolescents with Daily Headache (Chronic Daily Headache)
Ermonela Dokle,
Efigena Kabili,
Ina Gusho,
Adriatik Ramaj,
Florida Dobi
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
47-47
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.57
Downloads:
Views:
Abstract: Background: Mental health problems of the adolescents represent an issue not only for mental health professionals but also for the people involved in their education, caregivers and members of families. In the case of comorbid association between mental health disorders and medical conditions the severity of both disorders is amplified and a multidisciplinary approach becomes a priority in order to offer the best possible outcome.
Aims:Investigation of prevalence and correlation of comorbid psychiatric disorders in adolescents with chronic daily headaches (CDH).
Method: In the study were included 61 adolescents, age 14-19 years old, with daily headache, identified by neurologist and diagnosed for CDH in accordance with the ICD 10 criteria. Patients underwent a detailed psychiatric interview by a child and adolescent psychiatrist and were assessed using Beck Depression Inventory and Hamilton anxiety scale. The data were processed statistically with SPSS statistics 21.0.
Results and Discussion: 58 individuals (18M and 40F) competed the psychiatric evaluation. 24 subjects (47%) had more than one psychiatric disorder comorbid with major depression (21%) and with anxiety disorder (19%). Migraine associated with psychiatric disorders was frequently found compared with other primary headaches (odds ratio (OR) = 3.5, p = 0.002). Also psychiatric disorders were more frequent in the daily headaches over-utilization of analgesics.
Conclusion: The high frequency of comorbid psychiatric disorders in CDH, and statistical significance leads to the recommendation that CDH is not only neurologist's domain. Psychiatric evaluation needs to be asked frequently for children suffering from chronic daily headaches.
Abstract: Background: Mental health problems of the adolescents represent an issue not only for mental health professionals but also for the people involved in their education, caregivers and members of families. In the case of comorbid association between mental health disorders and medical conditions the severity of both disorders is amplified and a multid...
Show More
-

Frequency of Mental and Behavioural Disorders in Patients with Dementia
Ada Velo,
Iva Cajupi,
Ermela Shutina,
Ermonela Dokle,
Florida Dobi
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
48-48
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.58
Downloads:
Views:
Abstract: Background: Data from literature showed that both in early stages of neurodegenerative diseases and during their evolution, dementia symptoms are associated with other psychiatric disorders, such depression, or behavioural symptoms, agitation and aggression being the more frequent.
Aims: To detect the frequency of some psychiatric disorders in patients diagnosed with different types of dementia, resident in Tirana Region No.1.
Method: The study involved 257 people diagnosed with various types of dementia, from the neurologist or psychiatrist, resident in Tirana Region No.1. All subjects had done the neuroimaging assessment and a detailed psychiatric interview by psychiatrists of Mental Health Community Center No.1. Data were dropped in Microsoft Excel and processed with SPSS 12.1 program.
Results and Discussion: Psychiatric symptomatology it’s split into apathy, depression, aggressive behaviour and agitation. These problems were found after the visit of psychiatrists and it’s reflected in individual files of subjects that take part in the study. The diagnosis was established on the basis of DSM- IV criteria. Cases have been under medical treatment, and are followed in a dynamic way in the house by multidisciplinary center team formed by a psychiatrist, psychologist, social worker and nurse. Out of the total of 257 subjects diagnosed with dementia, 154 (60%) had degenerative dementia, 77 (30%) had vascular dementia and 26 (10%) had other dementia.
Conclusion: By the above-mentioned facts, we conclude that psychiatric symptomatology is dominant in all kinds of dementia. Diversity and their gravity it is depended on the stage of the disease and treatment received.
Abstract: Background: Data from literature showed that both in early stages of neurodegenerative diseases and during their evolution, dementia symptoms are associated with other psychiatric disorders, such depression, or behavioural symptoms, agitation and aggression being the more frequent.
Aims: To detect the frequency of some psychiatric disorders in patie...
Show More
-

Parental Perceptions about Autism Spectrum Disorder of Their Children: Impacts and Implications for Interventions in Albania
Eleana Naci,
Esmeralda Xhelilaj
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
49-49
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.59
Downloads:
Views:
Abstract: Aims: To identify and evaluate perceptions of parents of children with ASD at the time of diagnosis, and after receiving 2 years and 4 years ABA therapy.
Method: The participants of the study are parents of 150 children who receive diagnosis or receive treatment in 2 years and who receive treatment in 4 years at the Regional Center for Autism. The research method used is quantitate by using questionnaires. All these parents have fulfilled the questionnaires about the perception of the diagnosis and perception of ABA therapy, questionnaire about self-efficacy, depression, anxiety level, hopelessness, readiness for change. The other used questionnaires are, Beck's Depression Inventory, Hopkins list of symptoms, Parenting Self-Efficacy Test, Beck Hopelessness Scale and Jurica instrument of Prochaska and Di-Clemente.
Results and Discussion: Regarding the results of the study, as we expected, parental perceptions differ at the time of diagnosis, after 2 years, and 4 years of treatment. These differences were obvious regarding self-efficacy and parenting capacities, expectations from therapy, the willingness to change, emotional response from the situation, sense of hope. The main differences were found between the first group (time of diagnosis) and the second group (2 years of therapy), however we have found significant differences between all three groups mainly about expectations and sense of hope for the future, denial, despair, sense of guilt, family’s coping skills, family and social support, hope in the therapy etc.
Conclusion: We suggest that many factors might be the source for the differences that resulted including: cognitive and behavioural abilities of the autistic child, readiness for change, child age, existing parental problem, cohesion of the family. Further studies should be done in order to better understand how and the way these factors are integrated and influence parental perceptions.
Abstract: Aims: To identify and evaluate perceptions of parents of children with ASD at the time of diagnosis, and after receiving 2 years and 4 years ABA therapy.
Method: The participants of the study are parents of 150 children who receive diagnosis or receive treatment in 2 years and who receive treatment in 4 years at the Regional Center for Autism. The r...
Show More
-

Measuring Distress in Cancer Patients: A Cancer Distress Screening with a Cancer-specific Questionnaire
Kleda Mati,
Sonila Tomori,
Kleva Qeraj,
Erald Ruci,
Dhurara Tarifa
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
50-50
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.60
Downloads:
Views:
Abstract: Aims: To assess the psychological distress of cancer patients in a disease-specific manner as well as the demographic, social, financial and medical variables that have an impact on the distress.
Method: 115 patients were randomly selected from patients admitted for chemotherapy treatment in the Oncology Department, UHC of Tirana. Two questionnaires: 1-NCCN Distress Thermometer and Problem List for Patients and 2-Specific questionnaire regarding patient`s financial status were administered to all the patients.
Results and Discussion: Patients with unmet needs showed significantly higher psychological and symptom distress for most needs. From the explored demographic factors (gender, residence, age, and education), only age has a main effect upon depression (depression increasing with age), while education is the only factor from those analysed, which has a moderator effect. Regarding the analysed intra-individual variables, only dysfunctional attitudes, emotion-focused coping, and lack of emotional support from the family have main effects upon the level of depression (i.e., higher levels of dysfunctional attitudes, emotion-focused coping, and loneliness are associated with higher levels of depression), while neither of them has a moderator effect on the relationship between knowing the diagnosis and depression. We also found that financial distress was associated with overall distress.
Conclusion: Cancer-specific distress questionnaires give a more precise insight into patients' experience than general or psychiatric questionnaires. Coordinated psychosocial care may benefit cancer patients with significant distress. NCCN tool helps to assess the severity of patients’ distress and to determine the need for intervention.
Abstract: Aims: To assess the psychological distress of cancer patients in a disease-specific manner as well as the demographic, social, financial and medical variables that have an impact on the distress.
Method: 115 patients were randomly selected from patients admitted for chemotherapy treatment in the Oncology Department, UHC of Tirana. Two questionnaires...
Show More
-

Atypical Presentation of Celiac Disease in a Girl with Epilepsy and Retinopathy – Albanian Case
Aferdita Tako,
Mira Dervishi,
Sonila Tomori,
Aida Bushati,
Paskal Cullufi
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
51-51
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.61
Downloads:
Views:
Abstract: Aims: To report a case with celiac disease in a girl presented with epilepsy, behavioural disorder and retinal dystrophy.
Method: E.B. was hospitalised at age 11 with convulsive seizure (the third in a year) and irritable mood, hyperactivity, school refusal and eating problems. She was born in term with APGAR score 9/10 and weight 2800 gr. Her infancy and early childhood passed normally besides being a picky eater, not an easy child to obey and sleeping difficulties. When she got 8 years started to have decreased in vision, sleep disturbances, irritable mood and an iron deficiency anaemia was present. A year later she suffered night blindness and was diagnosed with conic retinal dystrophy. The molecular biology test resulted negative. At age 10 she had her first convulsive seizure early in morning as left hemi convulsion generalised secondarily. Her sleep patterns were dominated by sleepwalking episodes mostly around 2 hours after falling asleep associated with fear and psycho-motor agitation. She started to have nightmares and inability to remember these episodes. MRI scan without contrast resulted normal and she started treatment with carbamazepine 400 mg/daily. Five months later she had her second convulsive seizure with the same convulsive pattern: starting as hemi convulsion and afterwards generalised secondarily. EEG resulted in diffuse slow waves at fronto-temporal region. Gastrointestinal symptoms were constipation and abdominal discomfort.
Results and Discussion: Laboratory tests showed the following:
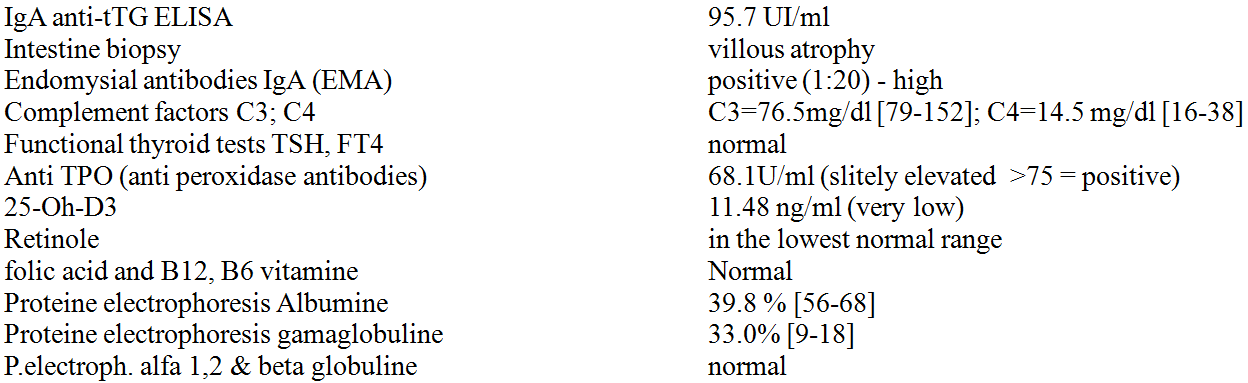
It was confirmed celiac disease and she started a gluten free diet and continued anti-epileptic medication switched to valproic acid. Immunoglobulin 100% IgG (Intratec) I/V was given during hospitalisation 2gr/kilo/day in 5 consecutively days.
Conclusion: Celiac disease has intestinal and extra-intestinal manifestations, caused by immune alterations or by nutrient malabsorption. The ophthalmic symptoms are rare within the extra intestinal manifestations, but should be investigated in patients with celiac disease and taken into consideration as the first systemic manifestations of the disease. Epilepsy, vitamin D&A deficiency, ophthalmologic manifestation in celiac disease are strongly correlated with an autoimmune pathway. Important for treatment consideration are gluten free diet, oral retinol and vitamin D daily, antiepileptic drugs and immunotherapy.
Abstract: Aims: To report a case with celiac disease in a girl presented with epilepsy, behavioural disorder and retinal dystrophy.
Method: E.B. was hospitalised at age 11 with convulsive seizure (the third in a year) and irritable mood, hyperactivity, school refusal and eating problems. She was born in term with APGAR score 9/10 and weight 2800 gr. Her infan...
Show More
-

Deinstitutionalizing Mental Health in Albania, Shortcoming of a National Reform
Erinda Bllaca,
Adrian Kati
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
52-52
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.62
Downloads:
Views:
Abstract: Our goal was to examines the right to quality mental health services in Albania from a comparative approach integrating the analysis of inherited clinical concept of psychiatric treatment with the “innovative” model of community based services, introduced after law amendments in 2012.
The Albanian health care system of the ’90s showed many challenges in splitting the clinical psychiatry into mental health and psychiatry (seen separately as a medical specialty). This was reflected in the difficulties of amending the 1996 law on mental health, and the urgency of the integration of concepts of human rights and fundamental freedoms for the treatment of people with mental illnesses. The adoption of the Convention on the Rights of Persons with Disabilities (CRPD, 2006) provided momentum to highlight the importance of the nexus between disabilities, mental health and deinstitutionalization.
Furthermore, the new context of the 2012 legislation, followed by secondary acts, action plans and strategies conceptualized a model of community care support which still needs time to be “digested” by the inherited excessively hospital-based system, which turned every person with problems into a prisoner, abide by prison-like rules, living in worse-than-prison conditions, having committed no crime.
Without immediate and continuous therapy and rehabilitation, limited [or no] freedom to exercise socio-politico-economic rights, forced routines and lack of privacy depriving people of their dignity, many live in such poor conditions that could cause them irreparably physical or mental harm, or even inhuman and degrading treatment.
Abstract: Our goal was to examines the right to quality mental health services in Albania from a comparative approach integrating the analysis of inherited clinical concept of psychiatric treatment with the “innovative” model of community based services, introduced after law amendments in 2012.
The Albanian health care system of the ’90s showed many challenge...
Show More
-

Fibromyalgia Case – Psychiatric and Psychological Implications
Alberta Shkembi,
Genti Xhelili
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
53-53
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.63
Downloads:
Views:
Abstract: Fibromyalgia is a chronic health condition characterized by widespread musculoskeletal pain, multiple tender points on physical examination, generalized muscular aching stiffness, fatigue, non-restorative sleep pattern, cognitive dysfunction and mood disturbance. People with this kind of diseases might be developing fibromyalgia. In this group are included: Rheumatoid, Arthritis Lupus.
The child L.T was referred to our clinic for a serious acute knees ache. Family members informed us that the child has knees ache for about a week and difficulty in walking, but for about 3 years the child had been having frequent morning pain of legs lasted for 30 minutes. The objective examination shows that left leg articulation was hyperaemic. Laboratory tests resulted: PCR 38, Sediment 30mm\h and a diagnose of idiopathic juvenile arthritis was established and he started treatment with Naproxen and hydroxychloroquine. One year later the child showed up again complaining exhaustion and asthenia, sleeping difficulties, diffuse pain in the upper and lower body. During the objective examination, the articulations were normal but the child had pain in all of fibromyalgia spots. All laboratory examinations resulted normal. Then he was diagnosed with fibromyalgia and was referred to a psychologist for consultation. Patient started psychotherapy treatments for about 15 weeks with a positive outcome.
Fibromyalgia is a disease which negatively affects the quality of children’s life and the social and emotional welfare in its everyday functioning.
Abstract: Fibromyalgia is a chronic health condition characterized by widespread musculoskeletal pain, multiple tender points on physical examination, generalized muscular aching stiffness, fatigue, non-restorative sleep pattern, cognitive dysfunction and mood disturbance. People with this kind of diseases might be developing fibromyalgia. In this group are ...
Show More
-

Siblings of Autistic Children and Language Delay
Alma Babo,
Aferdita Tako,
Sonila Tomori,
Mira Dervishi,
Florida Dobi,
Aida Bushati
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
54-54
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.64
Downloads:
Views:
Abstract: Background: Autism is one of the neurodevelopmental disorders that has dragged the most of international attention of general public and research community during the last decade. Even in Albania has obviously been raised the sensitivity on that disorder.
Aims: to evaluate the developmental and difficulties in siblings of autistic children.
Method: In a paediatric setting, during January-June 2012, were evaluated 126 siblings of children previously diagnosed with autism spectrum disorder. Clinical evaluation, MCHAT, SCQ, ADI were used and the diagnosis were done by a child and adolescent psychiatrist based on DSM-IVR criteria.
Results and discussions: The total number of siblings considered “in Spectrum” results to be 9 in 126, the rest of sample resulted to present some type of developmental difficulties. This figure of siblings with ASD stands on top line/margin of reported levels from studies in hospital population. In actual sample (which by being small sample doesn’t allow a deep statistical analysis but it resembles the results of similar specialized centers in other countries) it was found the existence of language delay in 36% of unaffected siblings and resistance to change together with restricted interests were found in 67% of them.
Conclusions: Siblings of autistic children constitute a population considered “in high risk”. Language difficulties are common and subject of early intervention in siblings of autistic children.
Abstract: Background: Autism is one of the neurodevelopmental disorders that has dragged the most of international attention of general public and research community during the last decade. Even in Albania has obviously been raised the sensitivity on that disorder.
Aims: to evaluate the developmental and difficulties in siblings of autistic children.
Method: I...
Show More
-

Depression in Terminal Cancer Patients: A Comparative Study Between Males and Females
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
55-55
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.65
Downloads:
Views:
Abstract: Background: Health care staffs such as psychologist and doctor are always trying to find ways for terminal patients to feel more comfortable as possible but also for them to alleviate pains and mental issues. In Mother Theresa Hospital in Albania working with patient in phase V terminal cancer was observed a distribution between genders with depression elements. There is a correlation between physical conditions, mental conditions, psycho-somatisation that has a big impact in phase V terminal cancer patients because of deterioration of general condition. Our hypothesis was “In terminal cancer patients phase V, more women suffer from depression than man”.
Method: We asked 100 patients in phase V terminal cancer, 50 males and 50 females and average age 50 years old that were diagnosed and treated in University Hospital Center “Mother Theresa” Tirana, Albania. They also were evaluated from our psychologist and psychiatrist and offered them psychological counselling during which they were administrated the Beck Depression Test Inventory (BDI). The BDI test contains 21 questions with multiple choices and is one of the most widely used psychometric test for measuring the severity of depression.
Results and discussions: The results for our work were meaningful. 32% of men compared to 14% female scored minimal depression; 16% of men compared to 4% female scored mild depression; 30% of men compared to 34% females scored moderate depression; 22% of man compared to 48% of females scored severe depression.
Conclusions: The results mean in relation to the study’s purpose. More females than males scored higher in the depression scale, correlating this with biological factors such as hormone factors, menopause etc.; social factors such as society, family and children the sense of not caring anymore; the higher level in experiencing physical and mental situations such as pain and the desire to end it. But this doesn’t underestimate depression level in males and the way they experience it.
Abstract: Background: Health care staffs such as psychologist and doctor are always trying to find ways for terminal patients to feel more comfortable as possible but also for them to alleviate pains and mental issues. In Mother Theresa Hospital in Albania working with patient in phase V terminal cancer was observed a distribution between genders with depres...
Show More
-

Epidemiology of Celiac Disease in Children in Albania and Psychological Implications of the Disease
Ermira Dervishi,
Aferdita Tako,
Virtut Velmishi,
Agim Gjikopulli,
Sonila Tomori,
Laurant Kollcaku,
Paskal Cullufi
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
57-57
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.67
Downloads:
Views:
Abstract: Aims: to describe the most recent data on the epidemiology of celiac disease in paediatric patients in Albania.
Method: 44 patients diagnosed with celiac disease (based on ESPHAGAN's criteria) during 2011-2013. The diagnosis was established using serological testing, level of tTG antibodies (IgA) as well as the degree of mucosal lesions through duodenal biopsy using endoscopy of upper gastro-intestinal tract. March classification was used to evaluate degree of histological changes in the small bowel.
Results and discussions: we had 26 girls and 16 boys, age interval 1-15 years, mean age for girls was 5,80 (1,1-13,8) and for boys was 6,09 (1,8-14,0). Symptoms presented were as follows: 38% had growth and developmental delays, 20% chronic diarrhoea, 11% abdominal pain, 7% vomiting, 4.5% anaemia, 3% abdominal distention, 2.2% chronic constipation, 2,2% irritability (asthenia) and 11% other symptoms. One in four patients had other associated disorders such as diabetes mellitus type 1 (n=4), genetic syndromes (n=2), autism spectrum disorders (n=2), hypothyreosis (n=1), IGF1 deficit (n=1). Mean value for tTG-IgA in girls was 137,8% (1,0-800) and in boys was 120,1 (2,0-369,). The histology of small bowel was consistent with March classification: T1-11,3% T2-18,18%, T3a- 20,4% T3b-9,0%, T3c-2,27%. The biopsy was not performed in 38.6% of entire sample. A positive correlation between morphological degree of changes and the level of tTG-IgA was found. High degree of March lesions was associated with high levels of antibodies tTG-IgA. All children were put in gluten-free diet. The follow up was done by evaluating weight, height, and level of tTG-IgA one year after being in gluten free diet.
Conclusions: Presentation with non-specific symptoms or a lack of symptoms is common and for early identification of celiac disease it is necessary serological testing in at risk groups.
Abstract: Aims: to describe the most recent data on the epidemiology of celiac disease in paediatric patients in Albania.
Method: 44 patients diagnosed with celiac disease (based on ESPHAGAN's criteria) during 2011-2013. The diagnosis was established using serological testing, level of tTG antibodies (IgA) as well as the degree of mucosal lesions through duod...
Show More
-

Migratory Trends of Psychiatric Residents in Albania - EFPT Brain Drain Project
Sonila Tomori,
Mariana Pinto Da Costa,
Tove Mogren
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
58-58
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.68
Downloads:
Views:
Abstract: Aims: Assessing the migration profile and migratory trends of psychiatry trainees in Albania as part of EFPT Brain Drain study in Europe and comparing it to other countries.
Method: Data collection was accomplished by an anonymous online survey and hard-copy questionnaire in University Hospital Center "Mother Teresa", to all psychiatric residents in Psychiatric Clinic in Tirana, during May-October 2013. Meanwhile this semi-structured questionnaire was circulated in 32 others European countries and was completed by 2281 psychiatric trainees between 2013 and 2014. Data has been analysed using the Software Package for Social Sciences for Windows v. 22.0 (SPSS Inc. Chicago, IL).
Results and discussions: More than 2/3 of Albanian respondents are very dissatisfied with their income but the main reasons for leaving the country are personal and family composition. A minority did have a short term or long-term experience abroad respectively 8,3% and 16.7% during which 50% of them considered to have the same opportunities as the locals. It resulted that 15% of all psychiatry trainees across Europe were immigrants. The countries with highest number of immigrants were UK, Switzerland, Germany and Sweden. Approximately one in twenty trainees across Europe had the perception of feeling discriminated or not having the same opportunities as the native trainees, especially concerning the work opportunities (55%) and academic conditions (45%), social conditions (42%). Around 60% of psychiatry trainees showed a high migratory tendency.
Conclusions: Losing large numbers of skilled psychiatrists contributes to decrease of the quality of mental health services. Albania needs to establish policies to promote returnees. Further research on feeling discriminated by immigrants workforce is necessary.
Abstract: Aims: Assessing the migration profile and migratory trends of psychiatry trainees in Albania as part of EFPT Brain Drain study in Europe and comparing it to other countries.
Method: Data collection was accomplished by an anonymous online survey and hard-copy questionnaire in University Hospital Center "Mother Teresa", to all psychiatric residents in...
Show More
-

Depression and Chronic Neuro-Inflammation – A Two-Way Street with a Possible Biomarker
Traian Purnichi,
Lavinia Duica,
Cristina Ruxandra Banu,
Mihail Cristian Pirlog
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
59-59
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.69
Downloads:
Views:
Abstract: Background: Nowadays, depression affects more than 300 000 million persons worldwide and it seems to be the main cause for disability by the World Health Organization report from 2017. The aetiology of depression seems to be heterogenous and remains uncertain.
Aims: In this context, no matter the depression form, the chronic neuro-inflammation and depression are linked by a bidirectional connection and this is important because in order to try to identify o biomarker for depression screening you need to research at the foundation of the disease.
Method: The data analysed are from a prospective study with N=100 patients who presented for laboratory routine evaluations between 1st February-30th June 2016 in the outpatient clinic of the National Institute of Gerontology and Geriatrics “Ana Aslan” (NIGG “Ana Aslan”), Bucharest, Romania. Depressive symptoms were evaluated using the Hospital Anxiety and Depression Scale (HADS). We used the recommended cut-off of ≥ 8 points for the HADS depression subscale. Laboratory data included all inflammation standard markers and serum high-sensitivity C-reactive protein (hs-CRP) determination for all the patients. The study was approved by the I.O.S.U.D. U.M.F. Craiova ethical committee. A written informed consent was obtained from all participants. Statistical Package for Social Sciences version 22 was used to analyse the data.
Results and discussions: In the study, we noticed a 63.4% of female, with a mean age of 71.6 (±7.51) years, from the urban area 92.7%. Moreover, 98.8% of people presented comorbidities. After controlling for somatic comorbidities, logistic regression model revealed that elevated levels of hs-CRP increased the likelihood of being diagnosed with depressive symptoms in elderly patients (β = .174; SE of β = .059; p = 0.003; 95% CI = 1.061-1.337). We found a relationship between higher levels of hs-CRP and increased risk for depression in older adults. That may be important as hs-CRP represents a vulnerability marker for cardiovascular diseases too. Using this marker may help to identify people at risk for both cardiovascular illnesses and depression.
Conclusions: The relationship between the 3 above variables is a complex one, since depression represents a risk factor for cardiovascular diseases and vice versa and hs-CRP seems to be a marker for both conditions. However, the cross-sectional nature of our study doesn’t allow us to clarify this relationship.
Abstract: Background: Nowadays, depression affects more than 300 000 million persons worldwide and it seems to be the main cause for disability by the World Health Organization report from 2017. The aetiology of depression seems to be heterogenous and remains uncertain.
Aims: In this context, no matter the depression form, the chronic neuro-inflammation and d...
Show More
-

Integration of Complementary and Alternative Medicine into Psychiatry - The Status Quo
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
60-60
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.70
Downloads:
Views:
Abstract: Background: In the era of evidence-based medicine, Complementary and Alternative Medicine is considered an outsider and its use is surrounded by controversies and preconceptions. Nonetheless, approximately half of the patients use it concomitantly with allopathic drugs without telling it to their physician.
Aims: To draw attention to this phenomenon for the benefit of the patients.
Method: Potentially relevant studies from 2010 to 2017 were identified from electronic databases.
Results and Discussion: The co-administration of nutritional supplements with psychiatric drugs may lead to toxicity or lack of clinical response due to pharmacological interactions. The use of phytotherapic compounds is not always safe due to toxicity of some active substances, contamination or low concentrations of active substance. Therefore, both patients and physicians should make an informed decision. Some substances like chromium, dehydroepiandrosterone, Rhodiola, inositol, S-Adenosyl-L-Methionine, omega - 3 have already proved some efficacy in the treatment of depression (by enhancement of the response to the conventional therapy).
Conclusion: Even use of Complementary and Alternative Medicine in psychiatry is still in its infancy, we have to keep an open mind as what is undemonstrated today may be explained tomorrow and the other way around.
Abstract: Background: In the era of evidence-based medicine, Complementary and Alternative Medicine is considered an outsider and its use is surrounded by controversies and preconceptions. Nonetheless, approximately half of the patients use it concomitantly with allopathic drugs without telling it to their physician.
Aims: To draw attention to this phenomenon...
Show More
-

The Importance of the Therapeutic Relationship in Diagnostic Acceptance in Patients with Psychosomatic Disorders
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
61-61
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.71
Downloads:
Views:
Abstract: Objectives: The objective of the study is to demonstrate the influence of the therapeutic relationship in diagnostic and therapeutic acceptance in patients with psychosomatic disorders, while identifying the obstacles that interfere between the patient and the physician, preventing the achievement of this goal.
Material and Method: We included 200 participants, 100 participants without psychosomatic damage (control batch) and 100 participants with psychosomatic disorders. The design of the study, carried out between 2008 and 2016, is part of the prospective and mixed studies; Quantitative and qualitative methods have been used concurrently and combined in the interpretation phase. We used three types of questionnaires (GPAQ, "The attitude to sickness scale", "Factors influencing patient satisfaction in relation to the doctor"). In the analysis of each of the branches, I structured syndromes with the criteria for the diagnosis of psychosomatic disorders DCPR (Diagnostic Criteria for Psychosomatic Research). The study complied with the principles of human studies.
Results: Applying the Cochran WG formula showed the following results for a 15% incidence of the phenomenon: p= 0,15; t=1,96; Δ = 20,05
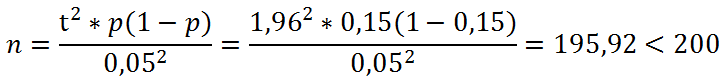
The analysis shows that the selected sample is representative of the proposed objective, namely: determining the validity of the hypothesis that the therapeutic alliance influences the diagnostic and therapeutic acceptance in patients with psychosomatic disorders. The correlation between the results obtained on the qualitative and the qualitative branch of the study confirms the working hypothesis namely: the therapeutic relationship influences the diagnostic and therapeutic acceptance in the patients with psychosomatic condition. An element of originality refers to the possibility of studying to perform affective prognosis, providing a way to anticipate respondents' choices using forecast charts. These offer the possibility to anticipate certain decisions that impact on the health of individuals in the future. Applicability in Clinical Practice: Modeling the correlation between the therapeutic relationship, somatization and the diagnostic acceptance that materialized in establishing the dependence between the human capital materialized in the therapeutic relationship, and the effectiveness of the medical act, completed by diagnostic and therapeutic acceptance (the element of difficulty in this category of patients).
Conclusion: The optimization of the therapeutic relationship (quantified by the patient's satisfaction index) increases the acceptance of diagnosis and therapy in psychosomatic patients.
Abstract: Objectives: The objective of the study is to demonstrate the influence of the therapeutic relationship in diagnostic and therapeutic acceptance in patients with psychosomatic disorders, while identifying the obstacles that interfere between the patient and the physician, preventing the achievement of this goal.
Material and Method: We included 200 p...
Show More
-

Child Depression
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
62-62
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.72
Downloads:
Views:
Abstract: The depressive disorder in children can be defined as a transitory stage of irritability or transitory depressive stage for at least one year, the certain diagnostic setting being done by adding two more depression symptoms that are present all the time, for at least half of the year under analysis.
The increase or decrease of the appetite, insomnia or hypersomnia, low level of energy or fatigue, low self-esteem, difficulties in focusing or making decision, feelings of uselessness are some of the frequent symptoms.
We tried to emphasize the role of the nurse in teaching the patient prone to depression about the long term risks of the disorders and the role of the behavioral interventions, as well as in training the social and interpersonal skills that may be of great help as treatment adjuvants.
Abstract: The depressive disorder in children can be defined as a transitory stage of irritability or transitory depressive stage for at least one year, the certain diagnostic setting being done by adding two more depression symptoms that are present all the time, for at least half of the year under analysis.
The increase or decrease of the appetite, insomnia...
Show More
-

Depression in Patients with Diabetes
Lavinia Alexandra Moroianu,
Eduard Polea Drima,
Alexandru Bogdan Ciubară,
Claudiu Ionuț Vasile,
Mihai Mutică,
Anamaria Ciubară,
Aurel Nechita
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
63-63
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.73
Downloads:
Views:
Abstract: Background: Comorbidity of depression - diabetes is a very important public health problem, both by increasing the consumption of medical services and the cost of health. Clinical care involves the development of effective strategies for recognizing depression and the implementation of personalized therapies according to the needs of each patient.
Aims: To introduce an objective approach for recognising early symptoms of depression in patients with clinical diagnose of diabetes and adapting treatment for each of them.
Method: There are two important theories on the occurrence of depression in diabetic patients: first, in which diabetic depression is the result of modified biochemical factors involved in the onset, exacerbation or remission of depression and diabetes, followed by a second hypothesis where depression is the result of psychosocial requirements imposed by diabetes.
Results and Discussion: Studies show that depression increases the risk of developing diabetes, but depressive symptoms are more common in patients with type I and type II diabetes with micro and macro vascular chronic complications. For people with diabetes and various depression diagnoses, the treatment can improve the quality of life and the glycemic level. Emotional problems associated with diabetes and / or chronic complications and the presence of atypical features of mood disorders in diabetic patients indicate that depressive episodes have a higher recurrence and longer duration of manifestation, with an increased incidence between the association of diabetes mellitus and the depression.
Conclusion: In Romania, patients with depression are stigmatized and on many occasions they do not ask for professional help. Different mental disorders such as depression are still underdiagnosed and not properly treated in different aspects (social, economic, cultural, intellectual) of people`s life with diabetes. Although obvious benefits have been demonstrated through an extensive interdisciplinary global approach of the treatment in diabetic patients, there are still many barriers for integrating all methods of treatment for depressive disorders.
Abstract: Background: Comorbidity of depression - diabetes is a very important public health problem, both by increasing the consumption of medical services and the cost of health. Clinical care involves the development of effective strategies for recognizing depression and the implementation of personalized therapies according to the needs of each patient.
A...
Show More
-

Objective Quantification of Psychomotor Disturbances in Patients with Depressive Episode
Svetlozar Haralanov,
Petya Terziivanova,
Evelina Haralanova
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
64-64
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.74
Downloads:
Views:
Abstract: Background: Psychomotor disturbances have been regarded as cardinal symptoms of depression for centuries and their objective assessment may have predictive value with respect to the severity of clinical depression, treatment outcome and prognosis of the depressive disorder. In clinical practice psychomotor disturbances are evaluated and measured subjectively – by clinical observation and/or by rating scales.
Aims: To introduce a novel objective approach for recording and measuring psychomotor activity and reactivity in patients with clinical depression.
Method: Psychomotor indicators of activity and reactivity were objectively recorded and measured by computerized ultrasonographic cranio-corpo-graphy.
Results and discussion: Objective and quantitative assessment of psychomotor symptoms may have pathophysiological significance as psychomotor disturbances go along with affective dysregulation. It is supposed that common neurotransmitter pathology in the brain structures causes simultaneously psychomotor and affective dysregulation that underlies the pathophysiology of depressive disorder. Also, psychomotor retardation is thought to be a cardinal depressive symptom in endogenous depressions – unipolar and bipolar. On the other hand, psychomotor agitation may be considered as latent bipolarity, although the presence of manic symptoms within a depressive state and the role of psychomotor agitation in depressive patients are still disputable.
Conclusion: Integration between different methods is needed in order to improve the understanding of psychopathology and neurobiology of a disputable diagnosis such as clinical depression. We introduce in the field of psychiatry an objective and quantitative approach, which could permit psychomotor discrimination not only between depressive patients and healthy controls, but also between subgroups of depressive patients.
Abstract: Background: Psychomotor disturbances have been regarded as cardinal symptoms of depression for centuries and their objective assessment may have predictive value with respect to the severity of clinical depression, treatment outcome and prognosis of the depressive disorder. In clinical practice psychomotor disturbances are evaluated and measured su...
Show More
-

Depression and Medical Conditions in a Screening Program
Bogdan Stania,
Mihaela Vladu,
Diana Clenciu,
Catalin Cotulbea,
Gabriel Oana,
Maria Lia Cara,
Mihail Cristian Pirlog
Issue:
Volume 5, Issue 6-1, November 2017
Pages:
65-65
Received:
10 October 2017
Accepted:
12 October 2017
Published:
13 October 2017
DOI:
10.11648/j.ajpn.s.2017050601.75
Downloads:
Views:
Abstract: Depressive disorder plays an important role in the evolution of associated somatic comorbidities, the most important of which being cardiovascular and cerebrovascular diseases, oncological diseases, neurodegenerative disorders, diabetes mellitus, or chronic liver disease. Presence of depression in individuals with somatic diseases could lead to non-adherence to the therapeutic program and pharmacological interferences, having as outcome a worsened evolution of all medical conditions.
Our results are parts of a multidisciplinary screening program developed between September 1st 2016 and December 31st 2017, in order to detect multiple medical conditions and depression. The study sample included 54 individuals (30 females, respectively 24 males), and their medical status was assessed through clinical and laboratory examinations. In order to detect presence of depression it was used Hamilton Depression Rating Scale.
Depressive disorder was identified in 16 subjects (29.63%), as following: mild depressive symptoms (HAM-D scores 8-13) were identified in 7 persons (12.96%), moderate depression (HAM-D scores 14-18) in 5 individuals (9.26%), while in 4 subjects (7.41%) HAM-D scores were over 19 – severe and very severe depression. Depression was associated with diabetes mellitus, respectively arterial hypertension in 14 subjects (25.93%), while liver steatosis was comorbid in 13 subjects (24.07%), and dyslipidemia in 12 individuals (22.22%). Moreover, for 9 subjects (16.67%), clinical data showed that they had a complex of all four medical and psychiatric diagnosis mentioned above.
Considering these elements and the risk induced by the presence of this pathological complex, it becomes important to develop and implement a multidisciplinary screening program in multiple settings, in order to detect and intervene in proper time for the treatment of depression.
Acknowledgments: Results were obtained in the framework of the implementation of the project Innovative Method of Prevention, Early Diagnosis, Monitoring and Treatment for Chronic Diabetic Disease, Major Cause of Morbidity and Mortality - MIPRED, code MySMIS 104769, ID P_38_313, implemented by INTERLAB MEDICAL, co-financed by the European Regional Development Fund under the Operational Program Competitiveness 2014-2020.
Abstract: Depressive disorder plays an important role in the evolution of associated somatic comorbidities, the most important of which being cardiovascular and cerebrovascular diseases, oncological diseases, neurodegenerative disorders, diabetes mellitus, or chronic liver disease. Presence of depression in individuals with somatic diseases could lead to non...
Show More































































